 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 16(3); 2014 > Article |
|
Abstract
Objective
Several studies have reported on the effectiveness of fronto-lateral craniotomy in reducing the operating time and post-operative complications. However, no study has practically evaluated this method from the cosmetic point of view.
Materials and Methods
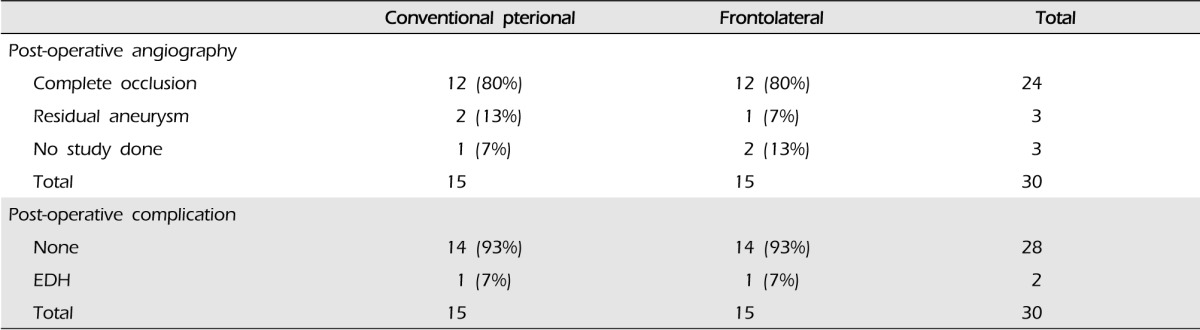
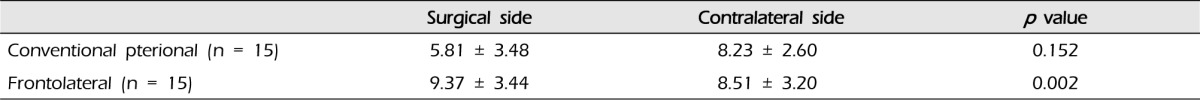
We designed this study for comparison of the clinical differences and cosmetic outcomes between the frontolateral craniotomy and the conventional pterional craniotomy for clipping of unruptured intracranial aneurysms. We performed a retrospective analysis of the two groups based on their medical records and radiologic findings juxtaposed with their length of hospital stay, intensive care unit day and operation time, and the emergence of postoperative complication, mean size of aneurysm, and temporal depression.
Results
After careful comparison of the thickness of temporalis muscle between the craniotomy side and the contralateral side, the results clearly showed that the conventional pterional craniotomy group was asymmetric by a p value of 0.152 and the frontolateral craniotomy group was symmetric by a p value of 0.002.
Conclusion
Frontolateral craniotomy could be a practical alternative for patients with an unruptured intracranial aneurysm in the anterior circulation including the posterior communicating artery, particularly those who are in a medically poor state or who highly demand minimal aesthetic mutilation.
The conventional pterional craniotomy (CPC), which was introduced and established by Yasargil in the 1970s, is the gold standard for approaching lesions in the sellar and suprasellar region, circle of Willis, sylvian fissure, and even the superior portion of the clivus and the basilar artery.8)9) However, with increased demands from surgeons and patients for a shorter operation time and a less invasive method for achievement of a better cosmetic effect without complications, several surgical approaches, including supraorbital eyebrow incision approach, mini-pterional approach, and frontolateral craniotomy (FLC), were recently introduced.2)3)7)
Several studies have reported on the effectiveness of FLC in reducing the operating time and post-operative complications. However, from the cosmetic point of view, this method has not been practically evaluated in any study. One of many cosmetic and functional complications of pterional craniotomy is temporalis muscle atrophy, which may hinder patients' rapid recovery and deter them from returning to their previous occupations.5) Therefore, we designed this study for comparison of the clinical differences and cosmetic outcomes between FLC and CPC for clipping of unruptured intracranial aneurysms.
From Aug. 2011 to Dec. 2013, clipping was performed in 283 unruptured aneurysm patients by a single surgeon in a single institute; FLC was performed in 15 cases. To verify the control group, we matched the age and sex and enrolled 30 patients through random selection. Patient randomization was performed using a random number generator available on the web (www.random.org). There were five males and 10 females in each group. Patients with multiple aneurysms of more than two or ruptured aneurysms were excluded from the study. We analyzed the two groups retrospectively based on their medical records and radiologic findings juxtaposed with their length of operation time, the emergence of postoperative complication, mean size of aneurysm, and temporal depression. The length of hospital stay was defined as a period of admission around surgery, including pre-operative evaluation.
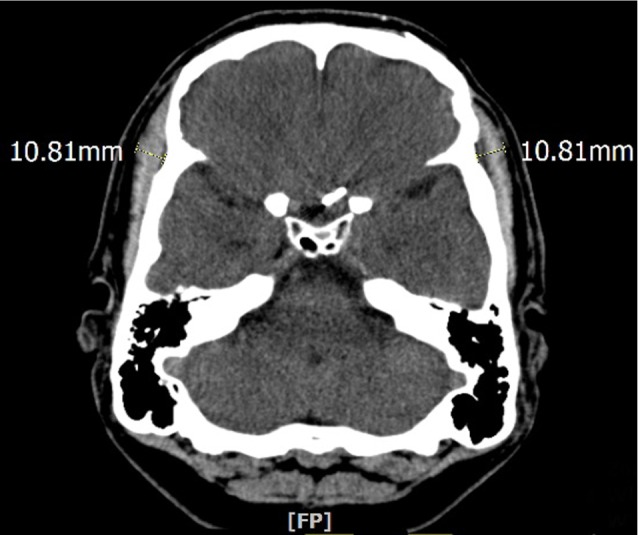
Due to possible temporal muscle atrophy, cosmetic effect after pterional craniotomy is not always satisfactory.3) Therefore, we compared temporal depression of the two different approaches. We first adjusted the contrast of brain computed tomography (CT) in order to have a better view of the soft tissue, and then measured the length of the thickest point of the soft tissue at the level of the sphenoid ridge (Fig. 2). Measurement was performed bilaterally, and the difference between craniotomy side and contralateral side was checked. All CTs were reviewed six months after the operation.
Operative technique of frontolateral approach
We followed the operative techniques as reported by Hernesniemi et al.3) The patient was in a supine position and the head was elevated above the cardiac level to minimize bleeding. The head was also fixed with three pins in the head frame (Mayfied) and was rotated 15-45 degrees towards the opposite side and tilted slightly depending on the precise location of the lesion. Minimal hair shaving was performed and the skin incision was short and behind the hairline (Fig. 1A). The one layer skin-galea-muscle flap was dislocated after its detachment from the bone by diathermy, thereby avoiding any possible injury of the branches of the facial nerve. The spring hooks were used to retract the flap anteriorly until the superior orbital rim was exposed. The temporal muscle was split only in its superior and anterior part (Fig. 1D). Only a single burr hole was placed posteriorly just below the insertion line of the temporal muscle (Fig. 1B). The bone flap was detached mainly by side-cutting craniotomy. The mean bone flap size was 4├Ś2.5 cm (Fig. 1C). After the dura mater was opened in a curvilinear incision pointing anterolaterally and elevated with stitches, the operating microscope was brought into place. After minimal opening of the sylvian fissure, careful dissection proceeded towards the aneurysm. Only one retractor was used for the brain dislocation. In closure, the bone flap was fixated with a skull fixator and a cranial plate (Fig. 1D).
As shown in Table 1, the mean age of the patients was 56.40 years old, while that for CPC and FLC was 56.53 and 56.27 years old, respectively. The mean operation time in the FLC group was 182.13 min, and 215.87 min in the CPC group. To clarify, the operation time was measured from the time of skin incision to closure. The length of hospital stay for both methods was 12.33 days, showing no difference. The location of the aneurysm also differed in the two groups. CPC was performed mainly on middle cerebral artery aneurysms (nine cases), followed by anterior communicating artery aneurysms (five cases) and anterior cerebral artery aneurysm (one case). On the other hand, FLC was most frequently performed on anterior communicating artery aneurysms (ten cases), followed by posterior communicating artery aneurysms (four cases) and anterior choroidal artery aneurysm (one case) (Table 1). For both approaches, there was a single occurrence of EDH as a postoperative complication (Table 2). Post-operative one-week angiograph follow-up (Table 2) showed two patients with residual aneurysm in the CPC group and one patient in the FLC group. However, no angiography was performed in one patient in the CPC group and two patients in the FLC group. For assessment of the aesthetic results, bilateral symmetry of temporalis muscle was measured by CT taken six months after the operation (Fig. 3). After careful comparison of the thickness of temporalis muscle between the craniotomy side and the contralateral side, the results clearly showed that the CPC group was asymmetric by a p value of 0.152 and the FLC group was symmetric by a p value of 0.002 (Table 3). In addition, a larger size of aneurysm was observed in the FLC group (Table 1). In measurement of maximum size of each aneurysm, mean size of the FLC group was 5.23 mm and that of the CPC group was 4.62 mm.
CPC was widely used and favored for many decades to access unruptured intracranial aneurysms at the anterior circulation.8)9) However, it has some notable disadvantages to consider as suggested by Herneniemi et al. These drawbacks include excessive drilling of the skull base, especially in the temporal region and the sphenoid wing, chances of cerebro-spinal fluid (CSF) leak, which can often lead to infection, optic or oculomotor nerve lesions, and possible injury of the upper branch of the facial nerve.3) In addition, epidural hematoma may be caused by CPC.3) Therefore, keyhole approaches such as supraorbital eyebrow incision approach, mini-pterional were introduced as an alternative, however, they have a limited operative working angle.2)4)7) Among them, FLC was determined to be the best, due to its advantages including shorter skin incision, smaller craniotomy, no alteration of temporalis muscle, which prevents temporalis muscle atrophy, and less complication such as postoperative epidural hematoma due to CSF leak.3) In addition, the size of the craniotomy is absolutely sufficient to reach the whole anterior part of the Circle of Willis, sellar, suprasellar legion and also the anterior part of the basilar artery if it is located superiorly from the posterior clinoid process (Fig. 2).3) However, some limitations were also reported. FLC offers less exposure of certain lesions that need to be exposed from a more lateral (temporal) perspective: posterior communicating artery aneurysms pointing posteriorly, anterior choroidal artery aneurysms, middle cerebral artery (MCA) aneurysms, and lower positioned basilar tip artery aneurysms.1)3) However, in our study, five out of 15 patients had posterior communicating artery aneurysms, which were all in the posterior direction.
Again, temporalis muscle atrophy is an aesthetic and functional complication of pterional craniotomy, which can delay patients' rapid recovery or deter them from returning to their previous occupations.5) The main factors causing muscle atrophy are 1) denervation, 2) loss of blood supply, 3) inappropriate muscle tension and 4) muscle fiber injury.6) When using FLC, the temporalis muscle is not manipulated during surgery, which not only shortens the operation time, but also discourages development of temporalis muscle atrophy. In this study, post-operative aesthetic outcome was proven to be significantly better in the FLC group than in the CPC group.
Our study showed that operation time for FLC tends to be shorter than that for CPC, with a similar rate of complication as CPC, a traditional method.
In both our surgical and clinical experiences, FLC proved to be superior to CPC by providing a safer and faster operation, with no post-operative temporal depression. Thus, FLC could be a pragmatic alternative for patients with an unruptured intracranial aneurysm in anterior circulation including posterior communicating artery, particularly those who highly demand a better cosmetic result.
References
1. Cha KC, Hong SC, Kim JS. Comparison between lateral supraorbital approach and pterional approach in the surgical treatment of unruptured intracranial aneurysms. J Korean Neurosurg Soc. 2012 6;51(6):334-337;




2. Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF, et al. The minipterional craniotomy: technical description and anatomic assessment. Neurosurgery. 2007 11;61(5 Suppl 2):256-264; discussion 264-65.


3. Hernesniemi J, Ishii K, Niemela M, Smrcka M, Kivipelto L, Fujiki M, et al. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 2005 94:17-21;


4. Mori K, Yamamoto T, Nakao Y, Oyama K, Esaki T, Watanabe M, et al. Lateral supraorbital keyhole approach to clip unruptured anterior communicating artery aneurysms. Minim Invasive Neurosurg. 2008 10;51(5):292-297;



5. Oikawa S, Mizuno M, Muraoka S, Kobayashi S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. Technical note. J Neurosurg. 1996 2;84(2):297-299;


6. Thompson N. Reconstructive Plastic Surgery. Philadelphia: WB Saunders; 1977. p. 293-300.
7. van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol. 1998 5;49(5):481-489; discussion 489-90.


8. Yasargil MG. Vertebrobasilar aneurysms. In: Yasargil MG, editors. Microneurosurgery. Stuttgart: Georg Thieme Verlag; 1984. Vol 2:p. 232-295.
Fig.┬Ā1
(A) Minimal hair shaving was performed and the skin incision was short and was behind the hair line; (B) Only one burr hole is placed posteriorly just below the insertion line of the temporal muscle; (C) The mean size of the bone flap was 4├Ś2.5 cm; (D) The temporal muscle is split only in its superior and anterior part. And in closure the bone flap was fixated with a skull fixator and a cranial plate.
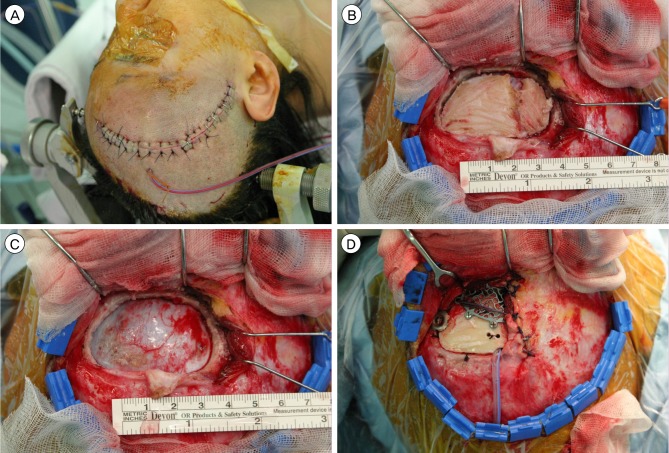
Fig.┬Ā2
The size of the craniotomy is absolutely sufficient to reach the whole anterior part of the circle of Willis, sellar, suprasellar legion and also the anterior part of the basilar artery if it is located superiorly from the posterior clinoid process.
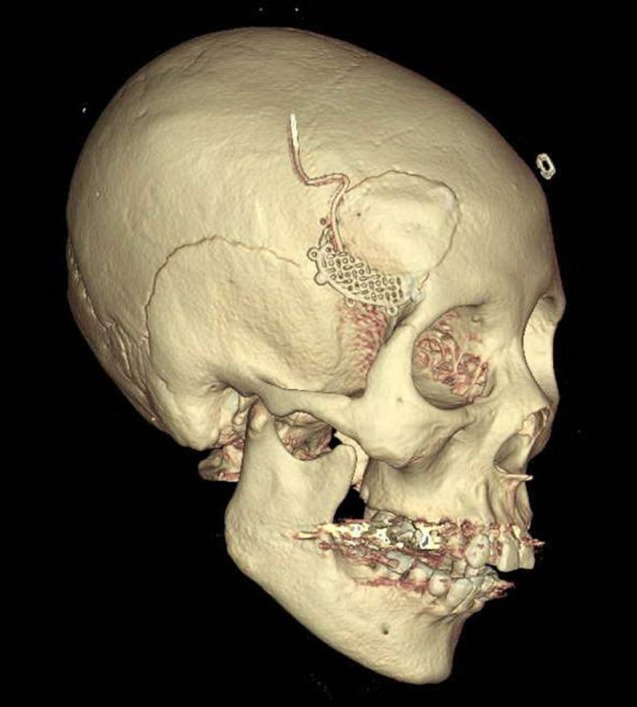
Fig.┬Ā3
Bilateral symmetry of temporalis muscle was measured through computed tomography taken six months after the operation.
- TOOLS
-
METRICS

-
- 3 Crossref
- 0 Scopus
- 2,177 View
- 28 Download
- Related articles
-
Trans-supraorbital Approach to Anterior Circulation Aneurysms.2000 March;2(1)


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



