Analysis of failed mechanical thrombectomy with a focus on technical reasons: Ten years of experience in a single institution
Article information
Abstract
Objective
Mechanical thrombectomy (MT) is an effective treatment for patients suffering from acute ischemic stroke secondary to large vessel occlusion. However, recanalization failure rates of interventions were about 20% in literature studies. We report our experience of unsuccessful MT with a focus on technical reasons.
Methods
From December 2010 to June 2021, six hundred eight patients with acute ischemic stroke due to large artery occlusion received MT using a stent retriever with or without an aspiration catheter in our institution. We divided the reasons for failure into six categories. We analyzed the reasons for failure by dividing our experience time into 3 periods.
Results
A total of 608 cases of thrombectomy for large vessel occlusion were identified in the study period. The successful recanalization rate was 90.4%. In most of the cases (20/57, 35%), the thrombus persisted despite several passes, and the second most common cause was termination of the procedure even after partial recanalization (10/57, 18%). Similar proportions of in-stent occlusion, distal embolization, and termination due to vessel rupture were observed. On analysis of three periods, the successful recanalization rate improved over time.
Conclusions
MT fails due to various reasons, and intracranial artery stenosis is the main cause of MT failure. With the development of rescue techniques, the failure rate has gradually decreased. Further development of new devices and techniques could improve the recanalization rates.
INTRODUCTION
Mechanical thrombectomy (MT) is a standard of care for acute ischemic stroke secondary to large vessel occlusion. Moreover, successful recanalization is an important factor for achieving the functional outcome. An increase in successful recanalization rates has improved stroke treatment and achieved a better outcome [3,13]. Meta-analysis has reported a successful recanalization rate of approximately 83%, whereas 17% of the interventions are unsuccessful [15]. There are many possible reasons for unsuccessful recanalization, from failed access to distal embolization, which are described in recent literature [9,18].
We retrospectively reviewed cases of failed MT over 10 years in a single institution. We also focused on the technical reasons for unsuccessful MT.
MATERIALS AND METHODS
A retrospective study was performed in 608 patients with acute ischemic stroke due to large artery occlusion who received MT between December 2010 to June 2021. The following data were collected: patient age and sex, along with a history of diabetes mellitus, hypertension, atrial fibrillation, dyslipidemia, coronary artery disease, malignancy, and smoking. Data on the procedure time, number of passes, and angiographic findings were also collected. Dyslipidemia was defined as a total cholesterol score over 200 mg/dL or a triglyceride score over 150 mg/dL. The final reperfusion score was rated based on the modified thrombolysis in cerebral infarction (TICI) grading scale. Failure of recanalization was defined as a score of 0, 1, or 2a on the modified TICI scale.
We divided the reasons for failure into the following six categories: 1) Failure of clot retrieval, 2) Partial recanalization (TICI 2a), 3) In-stent occlusion, 4) Distal embolization, 5) Termination due to vessel rupture, and 6) Distal occlusion with high risk profile. Failure of clot retrieval indicated failure of recanalization of main large vessel occlusion due to no change in the clot despite several passes. Partial recanalization indicated failure to reach TICI grade IIb or III although some branch vessels were recanalized. In-stent occlusion was defined as cases of failure due to thrombus formation after intracranial stenting. Distal embolization indicated that the main occluded large vessel was recanalized, but the distal small vessel (e.g. the M3 or M4 segment) was still occluded by distal emboli. Termination due to vessel rupture was defined as end of the procedure because of occurrence of vessel rupture during intra-procedure angiography, no matter how overcame. Distal occlusion with high risk profile referred to cases of only angiogram since distal occlusion (e.g. P2 segment of the posterior cerebral artery) unlike brain CT angiography.
In addition, we analyzed the reasons for failure by dividing our experience time into 3 periods.
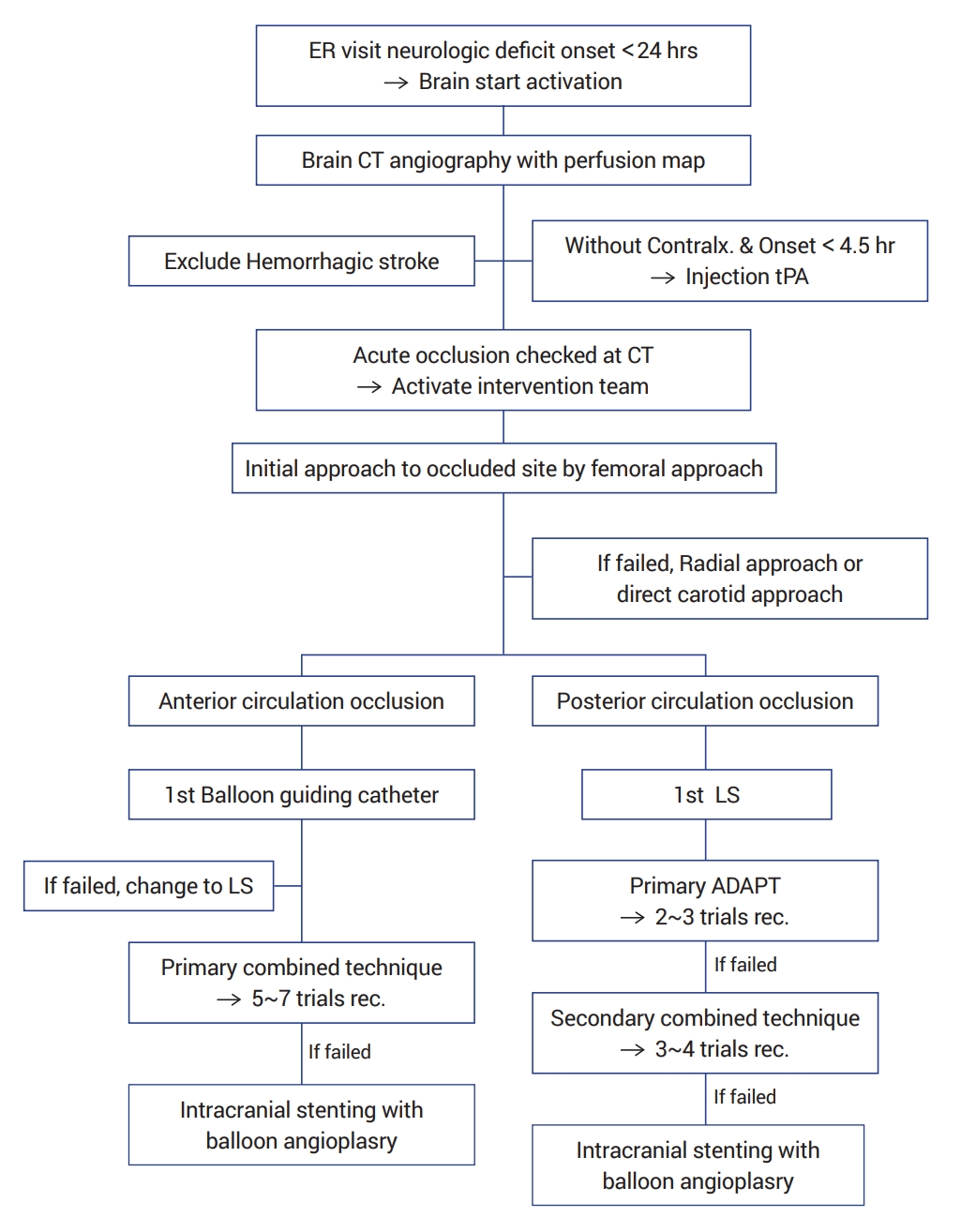
The period before the establishment of our institution’s protocol, before 2015, was called the pre-protocol period. The period of establishing the protocol was called the learning period and it ranged from 2016 to 2017 (Fig. 1). The period after 2017 was named the post-protocol period.
RESULTS
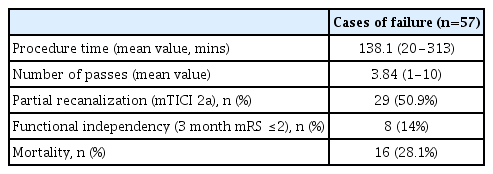
A total of 608 cases of thrombectomy due to large vessel occlusion were identified during the study period. Fifty-seven cases failed, and the successful recanalization rate was 90.4%. Demographic characteristics of patients with failed recanalization are presented in Table 1. The mean age of patients with failed recanalization was 71.5 years, and the number of male and female patients was similar (males n=28: females n=29). About half of the cases experienced dominant hemisphere stroke (29, 50.9%) and only 5 cases experienced posterior circulation stroke (8.8%). The mean value of the initial National Institutes of Stroke Scale (NIHSS) was 11.16 (range, 2-24). Radiologic and clinical outcomes are shown in Table 2. The mean procedure time was 138 minutes. The mean trial count was 3.8 times (range, 1-10). Twenty-nine cases showed partial recanalization (mTICI 2a). Only 8 patients (14%) achieved functional independence (3 months modified Rankin Scale ≤2), and 16 patients expired in 3 months.
During the whole period of MT, the most common reason for failure was difficulty of clot retrieval despite several passes (20/57, 35%). The second most common cause was termination of the procedure even after partial recanalization (10/57, 18%). Similar proportions of in-stent occlusion, distal embolization, and termination due to vessel rupture were observed (Table 3).
On analysis of the three periods, the successful recanalization rate improved over time. The success rate in the pre-protocol period was 82% (118/143), and 88% of patients were successfully recanalized during the learning period (116/132). Recently, in the post-protocol period, only sixteen patients showed undesirable results (success rate of 95%, 328/344).
The main reason for each period was different. Failure of clot retrieval was the most common reason in the pre-protocol period (13/25, 52%). However, similar proportions of failure of clot retrieval (5/16, 31%), partial recanalization (5/16, 31%), and in-stent occlusion (4/16, 25%) were observed in the learning period. Unlike before, during the post-protocol period, termination due to vessel rupture was the main reason for failure (7/16, 44%) (Table 4).
DISCUSSION
We analyzed the interventions from December 2010 to June 2021. During this period, we were able to confirm a successful recanalization rate of 90.4% in our institution. We analyzed in detail by the period, and we found that the successful recanalization rate was slightly increased during the learning period compared to the pre-protocol period. Also, the successful recanalization rate was increased by 7% from the learning period to the post-protocol period. As the protocol was established and the skill of the operator improved, the success rate increased dramatically.
Previously, Heider et al. published a categorized mechanism of unsuccessful thrombectomy. They reported that the main cause of thrombectomy failure was occlusion with peripheral ramifications (40%). Unlike in our study, which was the most common (35%) - not possible to make a proper comparison due to the different categories -, failure of clot retrieval was the second most common reason (25%). Compared with our report, they noted fewer cases of vessel rupture (3% vs 14%) [6].
The purpose of performing a review of failed cases is to overcome MT failure. We also tried to reduce failure in cases by using various methods and reported our experience. A history of thrombectomy can be called as a history of effort taken to decrease recanalization failure. To overcome refractory thrombectomy, several techniques and devices were published and developed. Recent advances in catheter technology have included very large, easily trackable, aspiration thrombectomy catheters that can more easily and reliably navigate the target vessel. Furthermore, the direct aspiration first pass technique (ADAPT) is a fast, simple, efficient, and safe strategy to achieve revascularization in patients with acute ischemic stroke secondary to large vessel occlusion [16]. The combination of aspiration and stent retrievers resulted in highly effective revascularization of large vessel occlusion in acute ischemic stroke patients [7].
Intracranial atherosclerotic stenosis could be the most common cause of refractory occlusion after MT in patients with acute ischemic stroke. Several previous studies have reported outstanding procedural and clinical outcomes of stent angioplasty using self-expanding stents [1,5,11,14,17]. It was reported that permanent stenting seems to be an effective and safe rescue treatment after failed MT [4,19].
To avoid parent artery rupture, more studies are needed to reduce vessel wall injury. It is necessary to understand the device and the changes in hemodynamic effects after the procedure. Vessel wall injury affects not only the outer diameter of the stent retriever but also the total radial force of the devices during the procedure [8]. Hemodynamic changes after the procedure can also affect vessel wall injury. Focal acceleration of blood flow velocities after MT may be a sign of endothelial layer disruption/intimal injury [12].
Urgent bypass surgery may also be an optional treatment for refractory occlusion. It has been reported that urgent bypass can prevent expansion of infarction and improve the clinical and radiological outcomes in highly selected patients [2,10].
Limitations
A comparison of failed cases with successful cases to evaluate the factors associated with failure was not performed. The study cohort was relatively small because it included patients at a single institution. Another limitation is that the study design was a retrospective review of case series.
CONCLUSIONS
There are various reasons for thrombectomy failure and we are overcoming them through multiple methods. Recently, vessel rupture has been the most common cause of thrombectomy failure in our institution, and more studies are needed to reduce vessel wall injury.
The development of new devices and techniques will also help reduce thrombectomy failure.
Finally, urgent bypass surgery may be an optional treatment for cases of thrombectomy failure.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.