Factors associated with rebleeding after coil embolization in patients with aneurysmal subarachnoid hemorrhage
Article information
Abstract
Objective
Aneurysmal subarachnoid hemorrhage (aSAH) has a high mortality rate, and hemorrhage amounts and perioperative rebleeding importantly determines prognosis. However, despite adequate treatment, prognosis is poor in many ruptured aneurysm cases. In this study, we identified and evaluated factors related to perioperative rebleeding in patients with aSAH.
Methods
The medical and surgical records of 166 patients that underwent endovascular embolization for a ruptured cerebral aneurysm at a single institution from 2014 to 2016 were retrospectively analyzed to identify risk factors of rebleeding. All patients were examined for risk factors and evaluated for increased hemorrhage by brain computed tomography at 3 days after surgery.
Results
This series included 54 men (32.5%) and 112 women (67.5%) of mean age 58.3±14.3 years. After procedures, 26 patients (15.7%) experienced rebleeding, and 1 of these (0.6%) experienced an intraoperative aneurysmal rupture. External ventricular drainage (EVD) (odds ratio [OR] 5.389, [95% confidence interval (CI) 1.171-24.801]) and modified Fisher grade (OR 2.037, [95% CI 1.077-3.853]) were found to be independent risk factors of rebleeding, and perioperative rebleeding was strongly associated with patient outcomes (p<0.001).
Conclusions
We concluded the rebleeding risk after aSAH is greater in patients with large hemorrhage amounts and a high pre-operative modified Fisher grade, and thus, we caution neurosurgeons should take care in such cases.
INTRODUCTION
Aneurysmal Subarachnoid Hemorrhage (aSAH) is a fatal disease with high mortality and morbidity rates. According to several studies, the mortality rate of aSAH ranges from 8% to 67% [18], and in particular, the mortality rate in patients that experience rebleeding is as high as 80% [14,15]. In addition to rebleeding caused by aneurysmal re-rupture, delayed bleeding that occurs despite complete treatment of ruptured aneurysm often increases mortality and the frequencies of unfavorable outcomes such as disability and morbidity. Therefore, it is important to be aware of the risk factors of rebleeding and to evaluate and predict the risks of rebleeding at admission. Larger aneurysm size, increased systolic arterial blood pressure on admission, and high Hunt-Hess grade on arrival have been reported to be associated with an increased risk of rebleeding, but the risk factors of rebleeding remain controversial [2,7,14,17,19]. Therefore, the purpose of this study was to evaluate risk factors of rebleeding after endovascular treatment for aSAH and to identify those useful for determining monitoring and management strategies after surgery.
MATERIALS AND METHODS
Patient selection and data collection
180 patients that underwent endovascular embolization with ruptured cerebral aneurysm by single neuro-interventionist at a single institution from January 2014 to December 2016 were studied retrospectively. All included patients underwent endovascular treatment within 6 hours after aneurysmal rupture. 14 patients were excluded from the study for the following reasons; 3 patients had deterioration of consciousness from preoperative brain computed tomography (CT) scan until immediately before surgery, 1 patient of confirming contrast leakage with rebleeding on procedural induced aneurysmal rupture during surgery, 1 patient of incomplete aneurysm coiling after endovascular treatment, 5 patients who were unable to perform subsequent brain CT scan because of unstable vital signs immediately after surgery, and lastly, there were 4 cases in which follow-up brain CT scans were not taken after surgery because the guardians did not want active treatment. So total 166 patients were enrolled in this study. We investigated age, gender, Hunt and Hess grade at presentation, aneurysmal size and location, preoperative Fisher and modified Fisher grades, intraoperative heparin loading, immediate postoperative external ventricular drainage (EVD) or lumbar drainage, and endovascular treatment techniques of all patients include in the study. In this study, the definition of rebleeding was defined as increased amount of subarachnoid hemorrhage (SAH), intracerebral hemorrhage (ICH), and intraventricular hemorrhage (IVH) on the follow-up brain CT scan performed 3 days after surgery compared to the brain CT scan performed immediately after surgery. Then, we examined whether there was an increased amount of bleeding on brain CT images taken immediately after surgery and 3 days after surgery compared to brain CT images taken immediately before surgery and analyzed the relation. This retrospective study was approved by the Institutional Review Board of Wonju Severance Christian Hospital (CR320164).
Endovascular procedure
In all patients, endovascular treatment was performed under general endotracheal anesthesia. Diagnostic digital subtraction angiography and embolization were performed using an angiography unit Allura Xper FD-20 (Philips medical, Eindhoven, NLD). Three-dimensional rotational angiography was performed in all 166 patients to confirm aneurysm size and shapes. 5000 IUs (international units) of heparin were loaded through a femoral sheath at the beginning of the procedures at surgeon’s discretion. During all 166 endovascular procedures, catheter flushing was maintained using a heparin/saline mix (5000 IU in 1 L of normal saline). Two surgeons who had performed the procedures were both neuro-interventionists with at least five years of experience. For each patient, the procedure techniques of single coiling, double microcatheter coiling, stent-assisted coiling and parent artery occlusion were determined according to the size and shape of the aneurysm. In all 166 cases, complete obliteration was achieved (Raymond–Roy occlusion classification class I). During the procedure, angiography was performed immediately after microcatheter positioning and coil insertion to check whether complications such as contrast leakage or thromboembolic event occurred. Patients were admitted to an intensive care unit (ICU) immediately after procedures and arterial blood pressure and electrocardiography were continuously monitored for at least a week. After surgery, in patients who underwent stent-assisted coil embolization were given dual antiplatelet medications (aspirin, clopidogrel) and only aspirin monotherapy was used in the patient who underwent simple coil embolization. Brain CT scan was performed immediately after procedures and 3 days later to check for rebleeding. Rebleeding was defined as an increase in the amount of SAH or the occurrence of new ICH, excluding contrast on follow-up brain CT scans.
Statistical analysis
The two-sample t-test or the chi-square test were used initially to identify associations with postoperative rebleeding, and logistic regression analysis was used to identify factors that independently predicted rebleeding and results are expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Quantitative variable results are expressed as means±standard deviations, and qualitative variable results as properties of variables. The analysis was conducted using SPSS (version 24.0. IBM Corp., Armonk, NY, USA), and statistical significance was accepted for p values <0.05.
RESULTS
Of the 166 total patients, 54 (32.5%) males and 112 (67.5%) females were enrolled, and the average age was 58.3±14.3 years. (range from 27 to 90 years). There were 121 (72.9%) patients with preoperative Fisher grade 4, and there were 54 (32.5%) patients with modified Fisher grade 2 and 65 (39.2%) patients with modified Fisher grade 4. Ruptured aneurysm size was average 5.9±2.8 mm. After the procedure, 26 patients (15.7%) showed an increase in hemorrhage on the follow-up brain CT scans, and one of them had aneurysmal rupture with contrast leakage during surgery. Table 1 summarizes the characteristics of the patients.
In the univariate analysis related to rebleeding, the age (p=0.601) and sex (p=0.506) of patients were not related, and the preoperative Glasgow Coma Scale (GCS) was lower in the rebleeding group (p=0.018). The Hunt and Hess grade was also higher in the rebleeding group at the time of admission to the emergency room (p=0.009), and the preoperative Fisher grade (p=0.011) and the modified Fisher grade (p=0.001) were higher in the rebleeding group. Aneurysm size (p=0.781), intraoperative heparin loading (p=0.782), and each endovascular treatment technique did not show statistical significance with rebleeding. However, the frequency of EVD (57.7% vs. 19.3%, p<0.001) and decompressive craniectomy after endovascular treatment (26.9% vs. 5.7%, p=0.003) was high in the rebleeding group. The frequency of unfavorable outcome was higher (73.1% vs. 30.0%, p<0.001) (Table 2).
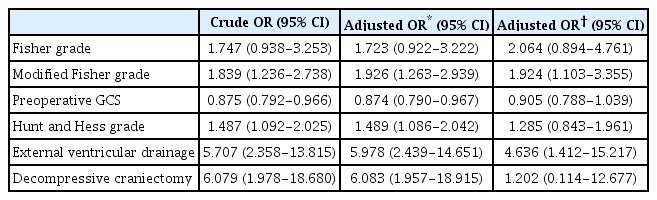
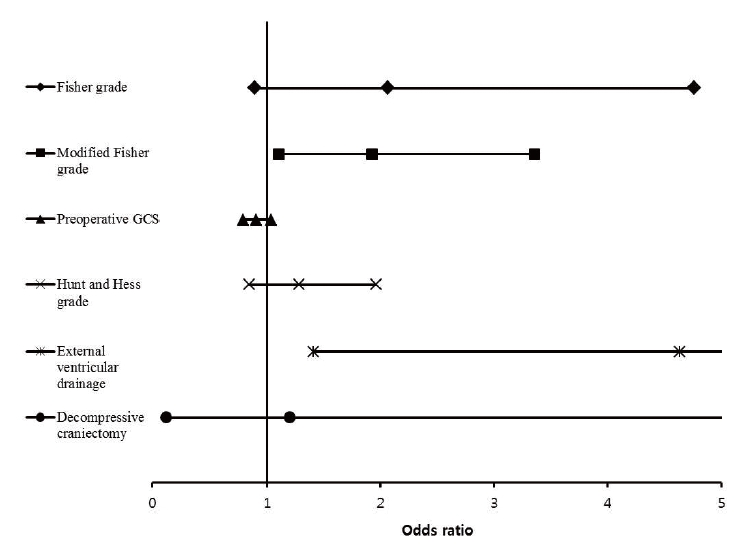
However, in the results of multivariate analysis, only modified Fisher grade was identified as an independent factor related to rebleeding as a preoperative factor (OR 1.924, 95% CI [1.103-3.355]), and as a factor after endovascular treatment, only EVD was confirmed as an independent factor related to rebleeding (OR 4.636, 95% CI [1.412-15.217]). On the other hand, Fisher grade, preoperative GCS, preoperative Hunt and Hess grade, and decompressive craniectomy were not related to rebleeding (Table 3) (Fig. 1).
DISCUSSION
ASAH is a fatal disease that causes high mortality and morbidity. According to several studies, the mortality rate has been reported between 8% and 67%, and the mortality rate in patients with rebleeding has been reported as high as 80% [14,15,18,21]. After the occurrence of aSAH, rebleeding varies not only from re-rupture in the ruptured aneurysm, but also from the increase in the amount of hemorrhage found after successful repair of the ruptured aneurysm. The incidence of rebleeding during the first 72 hours after SAH was reported was 8-23%, and about 50-90% of rebleeding occurred within the first 6 hours after primary bleeding [1,3,7,8,11-14,19,24]. In addition, even after the most ambitious treatment protocol for ruptured aneurysm closure after primary bleeding, rebleeding rates of up to 15% during the first 6 hours have been reported [14]. In most previous studies, rebleeding has been defined as the occurrence of newly developed intracranial hematoma after closure of aneurysm on brain CT scan after the first bleeding [4,23]. This includes remote hemorrhage as well as patients with re-rupture of aneurysms. In this study, rebleeding was also defined as a case in which hemorrhage amount increased on follow-up brain CT scan after completion of the treatment of aSAH ruptured aneurysm.
Risk factors of rebleeding after aSAH
The purpose of aneurysm occlusion after aSAH is to prevent rebleeding caused by re-rupture of the aneurysm. The mechanisms that cause rebleeding are complex and influenced by many factors. Although several studies have been conducted on risk factors that increase the risk of rebleeding of aSAH, not all studies have reported consistent conclusions, and for this reason, the risk factors related to rebleeding are still controversial [14]. van Donkelaar et al. [25] suggested that high World Federation of Neurosurgical Societies (WFNS) grade at hospitalization, large size aneurysm of 20 mm or more (adjusted harzard ratio (aHR) 4.4, 95% CI [1.6-13.2]), modified Fisher grade 3 or higher (aHR 4.7, 95% CI [2.1-10.6]) and EVD (aHR 1.7, 95% CI [1.4-2.5]) were reported as risk factors for aSAH rebleeding. On the other hand, Wu et al26). reported that when the cut off value of the cerebral aneurysm diameter was 7 mm, the risk of rebleeding was significantly increased in the group of 7 mm or more (19.4% vs. 6.8%, p=0.0487), but Fisher grade and WFNS score did not significantly increase the risk of rebleeding (p=0.6122, 0.4580). In the case of Hunt and Hess grades, some studies showed that the higher the grade, the higher the risk of rebleeding, while there were cases with insignificant correlation [12,14,17].
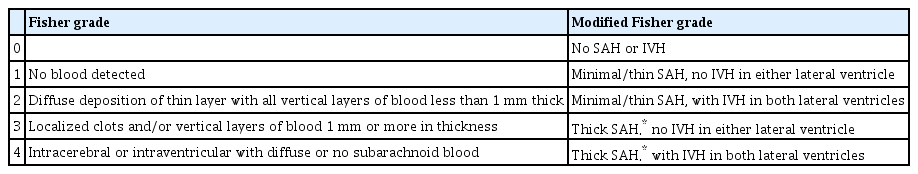
Fisher grade vs. modified Fisher grade
Fisher grade was first proposed by Fisher et al. in 1980, and radiologically grading the amount of hemorrhage present in cistern after aneurysmal SAH occurrence [5,6]. In general, Fisher grade has been widely used to evaluate the risk of delayed cerebral ischemia (DCI) because the amount of SAH present in cistern after aSAH shows the greatest correlation with the occurrence of DCI caused by vasospasm [5]. Fisher grade evaluates the risk of DCI through the amount of cisternal blood and the presence of IVH and ICH. If thick cisternal blood is shown, it is classified as Grade 3, and if ICH or IVH is present, it is classified as Grade 4, but the risk of DCI occurrence of ICH and IVH cannot be distinguished. Therefore, in 2001, Claassen et al. [5] reported that thick clot completely filling any cistern or fissure is the strongest risk factor for DCI and that the presence of IVH in both lateral ventricles has a strong correlation through a study on the possibility of DCI after aSAH. Also, based on the fact that the presence or absence of thick cisternal SAH and IVH acts as an additive risk factor for DCI, a modified Fisher scale was newly proposed according to the presence or absence of thick SAH and IVH (Table 4). In other words, it can be said that the modified Fisher grade reflects the amount of hemorrhage more accurately than the Fisher grade (Fig. 2).

(A) This patient had a small amount of SAH, but with IVH, and was classified as grade 4 for Fisher grade and grade 2 for modified Fisher grade. (B) This patient showed thick SAH without IVH and was classified as grade 3 in both Fisher and modified Fisher grades. (C) This patient was classified as grade 4 for both Fisher grade and modified Fisher grade as thick SAH with IVH. Compared with (A) and (C), although the absolute amount of hemorrhage shows a remarkable difference, the Fisher grade was all grade 4, and the difference in absolute hemorrhage amount was not distinguishable, but the modified Fisher grade was classified as grade 2 and 4, reflecting the hemorrhage amount. Compared with A and B, the absolute amount of hemorrhage is higher in B, but in Fisher grade, (A) was higher as grade 4, whereas in modified Fisher grade, grade increased as the amount of hemorrhage increases in the order of (A), (B) and (C). SAH, subarachnoid hemorrhage; IVH, intraventricular hemorrhage.
Ando et al. [1] proposed the hypothesis that the risk of rebleeding can be increased by interfering with the solidifying of blood clots when the aneurysm dome is embedded in the thick hematoma mass. and based on this, Ando et al. argued that the higher the modified Fisher scale, which is a measure that can intuitively reflect the amount of intracranial hematoma, is associated with the occurrence of rebleeding. In addition, van Donkelaar et al. [25] reported that the amount of blood acted as a surrogate marker of the defect size and stability of the ruptured aneurysm wall, showing a high correlation with the occurrence of rebleeding within 24 hours when the modified Fisher grade was 3 to 4 (aHR 4.7, 95% CI [2.1-0.6]). In addition, Hilditch et al. [10] reported a case of rupture of small pial branches of sylvian middle cerebral artery by expansion of sylvian fissure hematoma after acute post-aSAH, causing remote multifocal bleeding, resulting in the formation of hematoma in the sylvian subpial space. As a result, it was argued that there is a relationship between hematoma amount and remote hemorrhage, as the greater the amount of SAH caused by ruptured aneurysm, the greater the expanding effect of sylvian fissure and the likelihood of the occurrence of remote subpial bleeding will increase. Although these studies have different hypotheses, it can be said that they have in common argued the relationship between large amount hemorrhage and aSAH rebleeding.
EVD and rebleeding
Many studies have reported that SAH rebleeding is related to the extra ventricular drainage. In general, it is known that the hypothesis that rapid regulation of intracranial pressure (ICP) through EVD reduces the tamponade effect acting on recently ruptured aneurysm leading to rebleeding is the most reliable. This causes a decrease in ICP while cerebrospinal fluid (CSF) drainage through the EVD, which is known to increase the transmural pressure, which may exacerbate the risk of rebleeding. However, it is still not supported as solid evidence that CSF drainage increases the risk of rebleeding [9,14,16,20,22]. van Donkelaar et al. [25] reported initiation of EVD as a risk factor for rebleeding (aHR 1.9, 95% CI [1.4-2.5]). Similarly, Naidech et al. [17] reported whether EVD was implemented as a risk factor for rebleeding (OR 5.10, 95% CI [1.62-15.99]). but This study was limited to patients who were relatively good neurologic grade Hunt and Hess grade I to III at the time of admission, as a result, the authors said that it was a result with limitations in that it was not possible to exclude the case where EVD was performed because the patient worsened after the occurrence of rebleeding. In our study, it was concluded that the EVD implementation was related to rebleeding. However, in this institution, because EVD was performed when the large amount of hemorrhage or massive IVH was accompanied, the increase in risk of rebleeding becaused of the condition in which the amount of hemorrhage was high before EVD could not be excluded. Therefore, there is a problem in concluding that the rebleeding risk has increased by the implementation of EVD itself.
Limitations and strengths
This study is inherently limited by its non-randomized, retrospective, single center design and the relatively small number of cases included, which limit the generalizabilities of our findings.
On the other hand, since we performed ultra-early endovascular intervention within about 2 to 3 hours for all aSAH patients, rebleeding caused by aneurysm re-rupture that occurred between the initial brain CT angiography and the end of the intervention was excluded as exclusion criteria. Thus, it is a strength of this study that selective statistical analysis of patients with rebleeding, that is, remote hemorrhage, set in this study was possible.
CONCLUSIONS
If rebleeding occurs during aSAH treatment, it shows a high morbidity and mortality. For this reason, more careful monitoring and treatment are required in the case of the patient group with a risk factor associated with the occurrence of rebleeding after aSAH. According to this study, in the case of high modified Fisher grade on brain CT scan and accompanied by thick IVH requiring EVD, the risk of remote rebleeding after surgery is high. Therefore, more careful monitoring in the ICU is required during aSAH treatment.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.