An Unruptured Cerebral Aneurysm at the Origin of the Duplicated Middle Cerebral Artery
Article information
Abstract
A variety of cerebral vascular anomalies are widely applied, however anomalies of the middle cerebral artery (MCA) are relatively infrequent. The duplicated MCA (DMCA) is a MCA anomaly. Aneurysm arising from the origin of the DMCA is rare. Cerebral angiography in a 61-year-old female demonstrated a small (about 3 mm) saccular aneurysm located at the origin of the DMCA in the anterior direction. Considering the unusual location, the lesion was treated, regardless of the size. Aneurysmal characteristics of a broad neck and small size limited the endovascular approach, necessitating open surgery. Her postoperative course was uneventful and postoperative angiography showed complete obliteration of the aneurysm. The patient was discharged without neurologic deficit.
INTRODUCTION
The term middle cerebral artery (MCA) duplication was proposed for two vessels originating from the distal internal carotid artery (ICA).1)12) This has become widely accepted in describing duplicate MCA (DMCA). The reported frequency of DMCA is 0.2% to 2.9%, less than that of accessory MCA. Aneurysm formation at the origin of the DMCA is extremely rare, with only 28 clinical cases reported.2)5)8)10) Most cases of rupture have been small saccular aneurysms measuring less than 6 mm. We describe a case of a small unruptured saccular aneurysm arising from the origin of the DMCA.
CASE REPORT
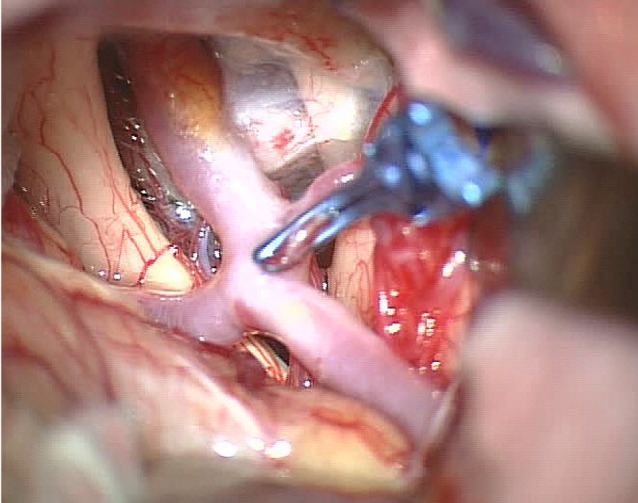
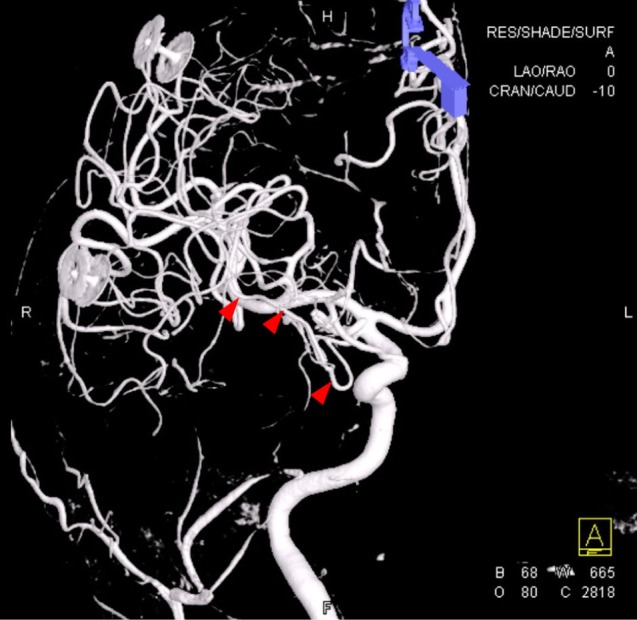
A 61-year-old female developed symptoms of left occipital area pain with shoulder tightness and tenderness. She had been diagnosed as hypertension 3 years ago. She visited the outpatient department of neurology because of a headache and underwent computed tomography angiography (CTA). The scan showed a small saccular aneurysm arising at the right distal ICA associated with an anomalous vessel (Fig. 1). The aneurysm measured approximately 3 mm size and had an anterolateral orientation. Three-dimensional rotational cerebral angiography showed an unusual vessel arising from between the right distal ICA and the anterior choroidal artery, coursing through the Sylvian fissure and a small aneurysm located at the origin of this unusual vessel (Fig. 2). The unusual location and hemodynamic stress, combined with the small size (3 mm) of the aneurysm prompted us to advise conservative management and observation. However, the patient was anxious about the aneurysm and desired aggressive surgical treatment. We complied. Initially, we considered an endovascular approach. However, the morphological features of a broad neck and small size limited this method, therefore open surgery was performed.

Preoperative CT angiography (CTA) showing an unusual vessel originating from the right distal ICA (arrowhead) and an associated small saccular aneurysm. ICA = internal carotid artery.
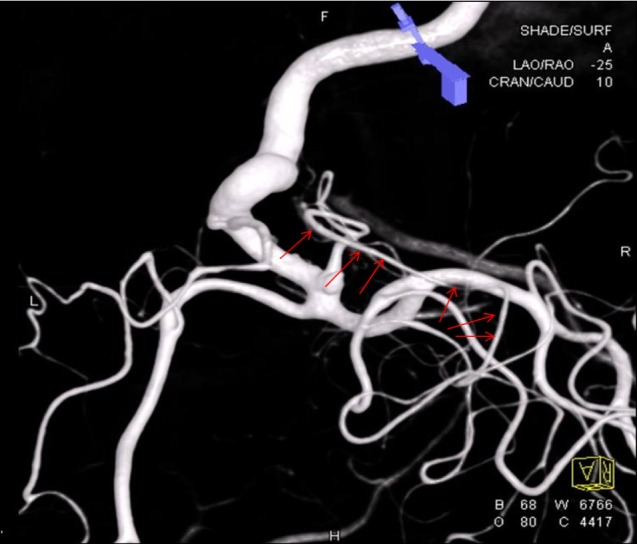
Preoperative oblique three-dimensional rotational cerebral angiography showing a vessel from the right distal ICA coursing parallel with other MCA branches to the Sylvian fissure and a small aneurysm. ICA = internal carotid artery; MCA = middle cerebral artery.
After craniotomy and dural opening, medial Sylvian dissection was performed. We were able to see the exact surgical field around the right distal ICA including the DMCA and aneurysm. The DMCA coursed laterally over the anterior temporal surface, and the aneurysm was bright red in color and pulsatile (Fig. 3). The aneurysm was clipped successfully and the patient recovered from general anesthesia without neurological deficits (Fig. 4). Postoperative 10 days, a follow-up cerebral angiography showed complete occlusion of the aneurysm and patent DMCA (Fig. 5). The patient was discharged. At the 6-month follow-up, the patient was neurologically intact and the headache was alleviated.
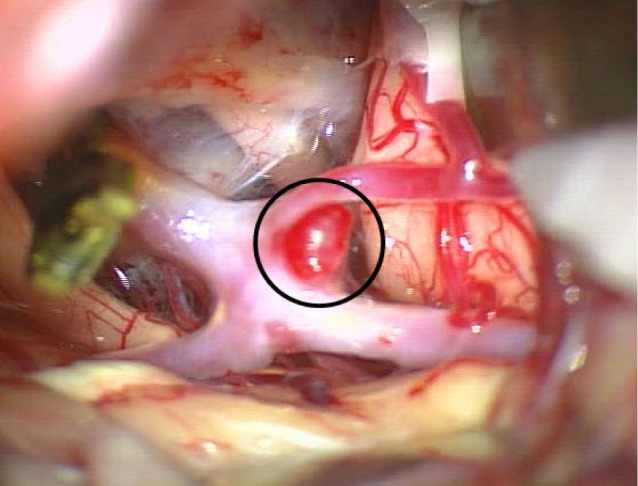
Intraoperative microscopic view showing detailed anatomy around the DMCA and aneurysm. DMCA = duplicate MCA.
DISCUSSION
The two most common anomalies of the MCA are DMCA and accessory MCA, but they are less frequently observed. The reported frequency of MCA duplication is 0.2-2.9% for that of the accessory MCA, which is 0.3-4.0%.3)4)9) Even on autopsy series they are found less than 3% of the time, and on cerebral angiography, the frequency is 1-1.5%.
Duplication of the MCA was first reported by Crompton in 1962, however the naming of this artery was initially confused.3) In 1973, Teal et al. defined the vessel arising from the internal carotid artery between the anterior choroidal artery and the terminal bifurcation of the internal carotid as a "duplicated MCA".3)11) They named the vessel arising from the anterior cerebral artery as the "accessory MCA". This terminology is now widely accepted. In this report, the authors used the term duplicated MCA (DMCA) in accordance with their definition. DMCA may contribute to the normal cerebral blood flow, and it may play a leading role in supplying collateral flow to the frontal lobe and the basal ganglia through the perforating arteries.7)12) Therefore, avoiding damage or occlusion of the DMCA during surgical manipulation is important.
According to Kai et al.,6) DMCA is classified according to two types; type A and type B. They noted that the type A DMCA separates at the top of the ICA, giving the impression of an early bifurcation. Type A DMCA may arise from the direct bifurcation of the MCA because the anomalous artery branches directly from the ICA. Type B originates in between the top of the ICA and the anterior choroidal artery, and has a smaller diameter than that of the main MCA trunk. Kai et al.6) suggested that type B DMCAs can expected to be subject to higher hemodynamic stress and that this could be a factor in the development of aneurysms on the type B DMCA.
Cerebral aneurysm associated with DMCA is rare considering the frequency of DMCA. Our report included only 28 clinical cases. Of these 28 DMCA aneurysms, 17 cases were ruptured and 11 were unruptured. Most of the ruptured ones were small saccular aneurysms measuring less than 6 mm. All aneurysms reported in the literature were associated with Type B DMCA and most were hemorrhagic and small in size (less than 6 mm). Our case was associated with type B DMCA and measured approximately 3 mm. Although our case was a small saccular aneurysm, we decided to treat this lesion due to its unusual location and abnormal hemodynamic stress as recommended by Kai et al.6) Its broad neck limited endovascular management as an initial approach. Direct neck clipping was planned. Some authors have proposed initial bypass surgery such as STA-MCA bypass to obtain adequate blood flow and to minimize ischemic insult in case of accidental occlusion of the DMCA during the operation. However, we were able to clip the aneurysm without difficulty and we think this procedure might be selected in the case of risk of DMCA damage through thorough preoperative evaluation. During the operation we identified a typical berry aneurysm with a bright red color and a fragile wall, indicating impending aneurysmal rupture. Through these findings, we think an aneurysm associated with DMCA has a high potential for rupture despite the small size. An aggressive approach once it is identified could be prudent.
CONCLUSION
This study reports on a literature investigation and clinical experience on a cerebral aneurysm found in a duplicated MCA.
Notes
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Portion of this work were presented in poster at the 28th Innovation in the Surgery for Complex Cerebrovascular Disease of Korean Society of Cerebrovascular Surgeons, Jeju, Korea, February, 6-7, 2015.