Surgical Recanalization of Distal Middle Cerebral Artery Occlusion Due to a Coil Migration During Endovascular Coil Embolization: A Case Report
Article information
Abstract
Coil migration into the parent artery during endovascular coil embolization is a rare, but life-threatening complication, which can induce thromboembolism and result in poor outcome. A 63-year-old man was referred to Chonbuk National University Hospital emergency center due to migration of a coil for a left middle cerebral artery bifurcation unruptured aneurysm. We performed an emergency craniectomy to remove the coil migrated to the distal M2 branch and thrombus, and aneurysmal neck clipping for his aneurysm. Fortunately, at the six month follow-up, the patient did not show any noticeable neurological sequela. In case of parent artery occlusion due to coil migration an immediate recanalization should be performed by a neurovascular specialist who can provide both surgical treatment and endovascular management in order to prevent severe sequela or even death.
INTRODUCTION
Since the introduction of the Guglielmi detachable coils in the early 1990s, endovascular detachable coil embolization has become one of the most preferred treatment modalities for intracranial aneurysms. However, some technical complications of endovascular coil embolization of intracranial aneurysms have yet to be overcome, such as intraprocedural aneurysmal rupture, thromboembolism, parent artery occlusion, and coil migration either during the procedure or after coil embolization. When such a complication occurs, immediate open surgery is required as soon as possible in order to save the patient from severe sequela or even death. We report on migration of a coil into the inferior branch of the middle cerebral artery (MCA), which was retrieved by craniectomy and arteriotomy. The coil migration occurred during an endovascular embolization performed for treatment of a MCA bifurcation aneurysm at a local medical center where no neurovascular surgeon is available.
CASE REPORT
A 63-year-old man was referred to Chonbuk National University Hospital emergency center because of a coil migration during endovascular coil embolization. He had received treatment for a left MCA bifurcation unruptured aneurysm at a local medical center. A neurovascular surgeon was not present at this particular medical center and the nearest hospital with one who could perform surgical management and endovascular management for such a patient with a coil migration complication was Chonbuk National University Hospital, which was located approximately two hours away from the local medical center.
At admission, he had stuporous mental status and right hemiparesis grade III. Initial brain computed tomography taken at the emergency center showed no intracranial hemorrhage, but showed a metallic object which appeared to be a migrated coil around the left insula (Fig. 1). Cerebral angiography performed at the local medical center showed a saccular aneurysmal sac, which measured 9.41 mm × 6.54 mm in size with a relatively broad neck of 4.38 mm at the left MCA bifurcation (Fig. 2). The coil part of coil embolization had detached from the aneurysmal sac and migrated to the left M2 inferior branch (Fig. 3). An emergency left pterional craniectomy was performed. After a left fronto-temporal opening, the left sylvian fissure was split and the MCA bifurcation was exposed. Following dissection of the sylvian fissure, the aneurysmal sac and M2 inferior branch were found, and the aneurysmal sac was in an unruptured state. After placement of temporary clips at the proximal and distal M2 inferior branch, the artery was incised, and the migrated coil and thrombus were visualized (Fig. 4A). The migrated coil and thrombus were removed gently and safely, and the arteriotomy vessel was repaired with 10-0 nylon (Fig. 4B). An intraoperative trans-cranial Doppler ultrasound confirmed the presence of distal flow in both M2 branches. The aneurysmal sac was clipped using a Sugita titanium #18 clip and a prophylactic decompressive craniectomy was performed (Fig. 5). The patient recovered from general anesthesia with mild dysarthria and right hemiparesis grade IV. Postoperative magnetic resonance diffusion-weighted imaging showed the acute cerebral infarction in the left M2 inferior division territory (Fig. 6A) and magnetic resonance angiography showed decreased blood flow in the left M1 distal portion, maybe due to a clip artifact (Fig. 6B). After 14 days, he was in stable condition with no aggravating signs of neurologic symptoms, therefore, he was discharged. At the six-month follow-up, the patient was neurologically intact.
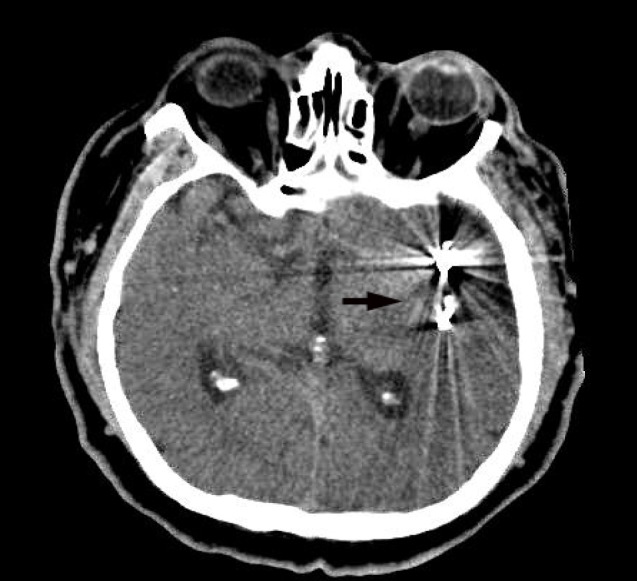
The initial computed tomography scan showing a metallic object which appears to be a migrated coil around the left insula (black arrow).

(A, B) Cerebral angiography showing a saccular aneurysmal sac, which measured 9.41 mm × 6.54 mm in size with a relatively broad neck of 4.38 mm at the left middle cerebral artery bifurcation.

(A, B) Cerebral angiography shows that the coil part of coil embolization has detached from the aneurysmal sac and migrated to the left M2 inferior branch (black arrow).

(A, B) Intraoperative field image showing a migrated coil and thrombus in the distal middle cerebral artery, and arteriotomy after removal of coil and thrombus.

Postoperative computed tomography shows the aneurysmal sac, which was clipped using a clip, and the presence of bony defect because of a prophylactic decompressive craniectomy (black arrow).
DISCUSSION
Since the introduction of Guglielmi detachable coils in 1991, endovascular treatment with detachable coils has been established as a mainstay therapy for intracranial aneurysms.6)12) With the development of neuroendovascular techniques, endovascular coil embolization has become a valid and increasingly used alternative to surgical clip obliteration in patients with intracranial aneurysms.9)17) However, despite increasing clinical experience and technical improvements, endovascular treatment still has inherent risks for morbidity and mortality.11) Several technical complications include intraprocedural aneurysmal rupture, thromboembolism, parent artery occlusion and coil migration, coil stretching, coil fracture either during the procedure or after coil embolization, and vasospasm of the parent artery. The most common complication of endovascular coil embolization for the aneurysm is thromboembolic event, which may result from poor technique, endovascular devices, and/or poor flushing of the catheter systems.11)14) Although coil migration into the parent artery is not a common event, it is one of the most feared complications that can occur during endovascular treatment of cerebral aneurysms and might be related to poor functional outcomes.2)4)13)15) Migration of coils or stents from their targets may be one of the most challenging complications of endovascular neurosurgery and contributes significantly to thromboembolic events when it comes to the endovascular embolization.8)
Development of remodeling devices such as stents and balloons has recently made endovascular coil embolization a popular treatment option for MCA aneurysm. Such a procedure has also provided equivalent angiographic results and showed an acceptable complication rate compared with aneurysmal neck clipping.7) Hence, compared with neurosurgical clipping, endovascular treatment should be the first treatment option for unruptured cerebral aneurysms in any location because it is cost-effective and has a lower morbidity and mortality rate.16) In addition, for patients with ruptured aneurysms judged to be technically amenable to both endovascular coiling and neurosurgical clipping, American Heart Association/American Stroke Association recommends that surgeons consider endovascular coiling as a preferred treatment option.3) Despite the worldwide popularity of endovascular treatment for intracranial aneurysms, surgical aneurysmal neck clipping is the primary treatment option for MCA aneurysms. Not only are they easily accessed in the surgical clipping approach, but also these aneurysms often have broad necks relative to the sac width and may partially incorporate one or both of the M2 branches into the aneurysm neck.7)
The patient was incidentally found to have an unruptured aneurysm on the left MCA bifurcation with a relatively broad neck during a health check-up. Even though the neck of the aneurysm was relatively broad, the decision was made to occlude it by endovascular coil embolization due to a large dome to neck ratio (> 1.5). However, a coil migration into the distal parent artery occurred during the embolization, especially for particularly broad-neck aneurysms. Possible causes include a size mismatch between the embolized coil and the caliber of the parent artery, inadequate position of the microcatheter within the aneurysm, mechanical vasospasm due to catheter manipulation in the early stage of the endovascular procedure,1)5)11) disuse of an assisting device like stent or balloon, and unskillful technique of an inexperienced operator. An emergency surgical operation for complications associated with coil embolization is uncommon,10) however, as mentioned above, coil embolization is still associated with fatal complications. Obstruction with migration of a coil into the parent artery may be particularly difficult to resolve with an endovascular procedure.13) Use of a coil retrieval device is a possible alternative, but this may require negotiating through the clot and may be associated with complications like perforation.10) Further endovascular procedures may risk pushing the migrated coil more distally, resulting in a more complex situation.
In addition, it has been reported that an open surgery could be the best option when endovascular procedures are difficult or unsuccessful.2)13) Coil embolectomy, vessel repair, and aneurysmal neck clipping are necessary for surgical treatment after such distal coil migration. However, removal of intravascular coils is not always possible due to adhesion to the arterial wall. In such a case, revascularization procedures such as superficial temporal artery-MCA bypass may even be necessary; therefore, it is important to preserve the superficial temporal artery when performing surgery.15)
CONCLUSION
For achievement of a successful endovascular coil embolization, selection of the right indication is essential and should be performed carefully because unexpected complication can occur during the procedure. Neurosurgical management is one of the most effective ways to revascularize parent artery occlusion by coil migration. In order not to leave any sequela associated with coil migration, rapid extraction of the migrated coil as possible is critical, and, for this reason, a skillful neurovascular specialist who can provide appropriate surgical management and endovascular management for such a patient with a coil migration complication can come in handy.

