 |
 |
| J Cerebrovasc Endovasc Neurosurg > Epub ahead of print |
Abstract
We report a case of a 24-year-old patient who presented after a head trauma with a traumatic occlusion of his left internal carotid artery. He underwent diagnostic cerebral angiogram and was found to have a direct left carotid-cavernous fistula (CCF) with retrograde filling from the posterior circulation across the posterior communicating artery. Because of the severe injury to the left internal carotid artery (ICA), reconstructive repair of the ICA was not possible. The patient underwent deconstructive repair of the CCF by coil embolization using a posterior retrograde approach. Coils were successfully placed in the cavernous sinus and back into the left ICA with complete cure of the CCF and restoration of cerebral perfusion distal to the treated CCF. We review the types of CCFs, their clinical presentation, and their endovascular treatments. Retrograde access of a direct CCF is rarely reported in the literature, and we believe this approach offers a viable alternative in appropriately selected patients.
Carotid-cavernous fistulas (CCF) are vascular shunts allowing blood to flow either directly, by way of ICA injury, or indirectly, from carotid artery meningeal branches, into the cavernous sinus [5]. Barrow classically defined 4 types of CCFs [1]. Type A CCFs are direct, high-flow lesions resulting from arterial wall tearing that connect the ICA and cavernous sinus [1,5]. They are the most common type of CCF and are often caused by trauma, as in the patient in this report. Aneurysmal rupture is another common cause. Types B, C, and D CCFs are indirect, low-flow lesions that arise from the meningeal branches of the internal carotid artery or external carotid artery [1,5]. The pathophysiology of both direct and indirect CCFs is related to increased pressure in the cavernous sinus resulting from the introduction of arterialized blood causing venous hypertension as well as changes in venous drainage [7]. Changes in venous drainage can occur anteriorly, posteriorly, contralaterally, or inferiorly but often take place in multiple directions simultaneously. They often present acutely with proptosis, chemosis, orbital bruits, visual disturbances, and headache [5]. Elevated intraocular pressure, intracerebral hemorrhage, and epistaxis also can occur [7].
While non-invasive diagnostic imaging such as including computed tomography angiography and magnetic resonance imaging can be helpful diagnostically8), diagnostic cerebral angiography (DCA) is the gold standard for diagnosis. DCA allows for the best characterization of CCF angioarchitecture, including fistula size, fistula location, characterization as direct or indirect, venous draining patterns, and high-risk features such as cortical venous drainage or the presence of a pseudoaneurysm [6,7].
DCA simultaneously allows for treatment planning. Endovascular transarterial or transvenous embolization is the first line treatment modality for most CCFs as carotid sacrifice risks ischemia of the cerebral territory supplied by vasculature arising from an internal carotid artery (ICA) [5,6]. Transarterial embolization is favored for direct CCF embolization, though it can be used for treatment of indirect CCFs [5,8]. Transarterial embolization for direct CCF embolization usually occurs using an antegrade approach via the common carotid and internal carotid arteries. Retrograde approaches to direct CCF embolization are very rarely reported [4,8] despite retrograde transvenous approaches being commonly used to access the cavernous sinus via the inferior petrosal sinus or the facial and superior ophthalmic vein for indirect CCF embolization [5,8] with metallic coils with or without liquid embolic agents [5]. Our case reports a rare retrograde approach to a direct CCF with an excellent angiographic outcome.
A 24-year-old male with no significant past medical history presented after an un-helmeted all-terrain vehicle accident. Proptosis of the left eye was noted on arrival, and intraocular pressure was elevated to 61 mm Hg. Computed tomography of the head demonstrated multiple left-sided skull fractures and showed multicompartmental intracranial hemorrhages (Fig. 1A-C). Computed tomography angiography of the head and neck showed poor opacification of the cervical and intracranial portion of the left ICA with delayed images showing a string sign to the level of the petrous segment (Blunt Cerebrovascular Injury IV) [2] (Fig. 1D). There was no evidence of an intracranial large vessel occlusion. He underwent emergent left decompressive hemicraniectomy.
The patient subsequently underwent DCA and was noted to have traumatic left ICA dissection leading to complete occlusion just distal to the origin (Fig. 1E). There was a direct left CCF [1], filling retrograde from the posterior circulation across the posterior communicating artery. There was also minimal supply from the left external carotid artery. Notably, anterior circulation intracranial vessel distal to the CCF were not observed, which suggested a steal phenomenon related to the CCF (Fig. 1F).
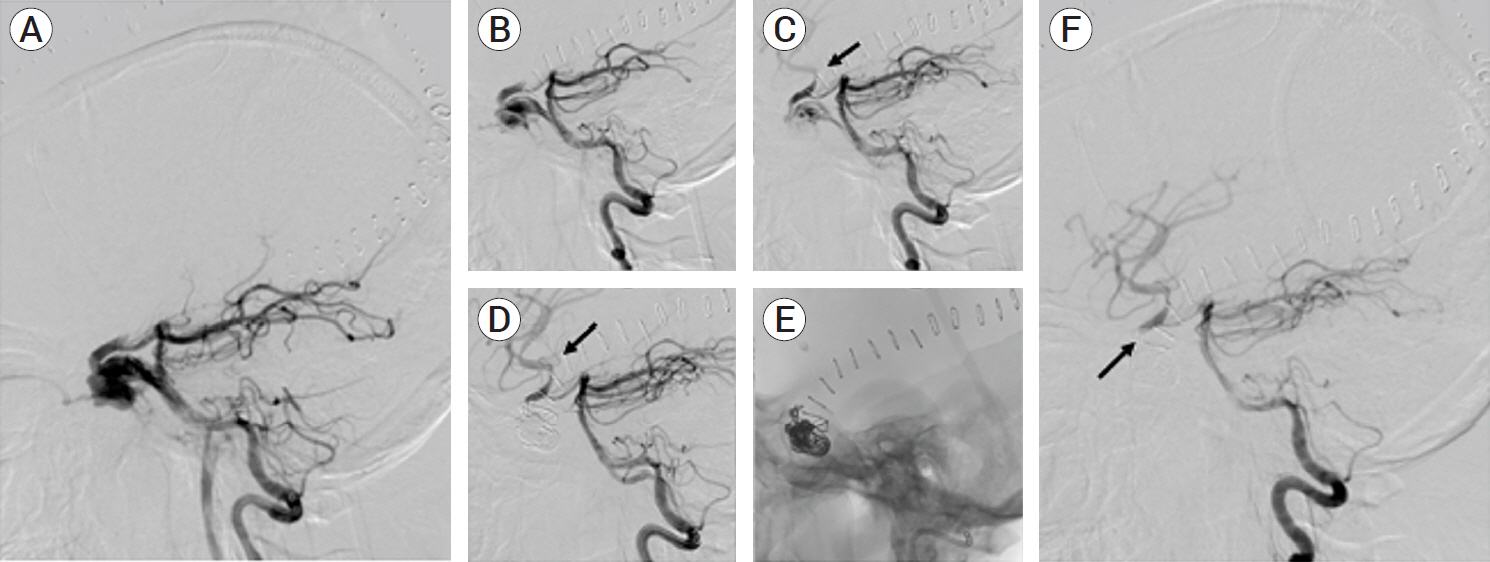
The patient underwent deconstructive repair of the CCF by coil embolization. Though direct CCFs are traditionally treated via an antegrade approach, a posterior access approach was chosen for this direct CCF because it filled by way of the posterior circulation. First, access to the left cavernous sinus was obtained by way of the posterior circulation. A Benchmark catheter over a 5 French Select catheter over a 0.035ŌĆ▓ŌĆ▓ Terumo guide wire were navigated to the distal left vertebral artery. Next, a SL10 microcatheter over a Synchro 2 microwire was inserted into the Benchmark and carefully navigated through the basilar artery, left posterior communicating artery, left ICA, then through the area of injury into the cavernous sinus. Smart 14├Ś60, Target 12├Ś30, 10├Ś40, 8├Ś30, and Smart 7├Ś25 coils were then placed in the cavernous sinus and back into the ICA (Fig. 2A-C). Special effort was made not to occlude the left anterior choroidal artery and to avoid vasospasm of the posterior communicating artery. After embolization, there was no residual arterio-venous shunting, and there was notable filling of anterior circulation intracerebral vessel distal to the CCF indicative of restored intracerebral perfusion in the anterior circulation (Fig. 2D, E). Follow up DCA 5 weeks later showed complete cure of a the traumatic left CCF after use of a retrograde approach (Fig. 2F).
Transarterial approaches require treating the CCF either through the ICA or the external carotid artery. Antegrade approaches are most often used, especially when treating direct CCFs. By advancing a catheter through the cervical carotid artery and into the cavernous ICA, operators can access the cavernous sinus and place metallic coils without or without liquid embolic agents into the cavernous sinus [5,6]. Success rates for direct CCFs have been reported as high as 94% [3].
While antegrade access of a direct CCF is common, retrograde arterial access of a direct CCF is very rarely reported [4,8]. In our case, antegrade approach was not possible because of the severe proximal ICA injury leading to complete occlusion. The ICA supply was retrograde from the posterior circulation by way of the posterior communicating artery, and the lack of filling of the anterior circulation suggested a steal phenomenon caused by the CCF. Retrograde approach allowed access to the cavernous sinus as well as treatment of the primary arterial contributor to the CCF. It also led to restoration of cerebral perfusion in the anterior circulation and resolution of the steal phenomenon by the CCF. We were able to avoid vasospasm of the posterior communicating artery, which can be a technical limitation [8,9]. This case illustrates that a retrograde approach can offer a viable alternative for direct CCF embolization when an antegrade approach is not possible.
Our case did have important considerations. As with all CCF cases, the decision to observe or treat must weigh the risks and benefits. In our case, observation could increase the risk of hemorrhage from CCF rupture, and the patientŌĆÖs multicompartmental hemorrhages precluded a safe trial medical therapy with antiplatelet therapy or anticoagulation. Treatment was thus felt to provide the patient with the best chance of recovery given his severe trauma. It was not possible to perform a reconstructive repair of the ICA given the severe proximal injury leading to complete occlusion. Endovascular repair was felt to be the safest option, and retrograde embolization of the patientŌĆÖs direct CCF was successful.
In this case report, we present the case of a traumatic left ICA dissection leading to left occlusion and a left direct CCF filling retrograde through the posterior communicating artery who underwent deconstructive CCF repair via a retrograde approach. Retrograde approach permitted cavernous sinus access in addition to endovascular treatment of the primary arterial contributor to the CCF as well as resolution of the steal phenomenon by the CCF and subsequent restoration of intracranial perfusion. Follow up angiography showed excellent angiographic result.
Fig.┬Ā1.
(A) Superior axial view of non-contrast computed tomography of the head showing multi-compartmental intracranial hemorrhage, including predominantly left frontal subarachnoid hemorrhage (arrow). (B) Inferior axial view of non-contrast computed tomography of the head showing extension of subarachnoid hemorrhage into basilar and quadrigeminal cisterns. (C) Axial computed tomography angiography of the head showing asymmetric contrast enhancement in the left cavernous sinus (arrow). (D) Sagittal view of computed tomography angiography of the neck showing occlusion of the left internal carotid artery (arrow). (E) Lateral diagnostic cerebral angiography with contrast injection in the left common carotid artery showing occlusion of left internal carotid artery distal to bifurcation (arrow). (F) Lateral diagnostic cerebral angiography with contrast injection in the left vertebral artery showing CCF filling via the left posterior communicating artery. CCF, carotid-cavernous fistula
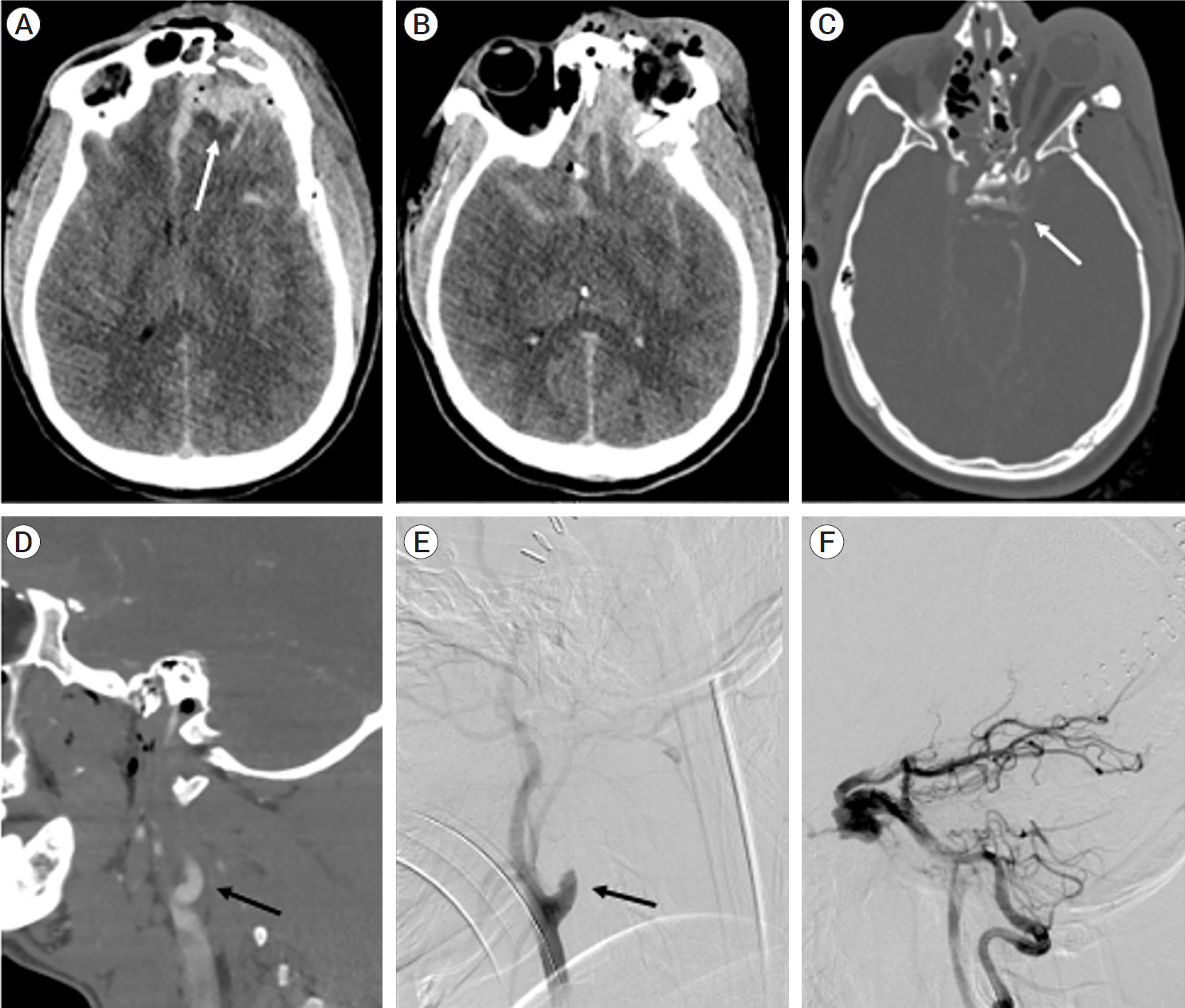
Fig.┬Ā2.
(A) Digital subtraction lateral view of left vertebral artery contrast injection showing CCF filling via the left posterior communicating artery. (B) Lateral view of left vertebral artery contrast injection after deployment of 1st coil via retrograde approach. The microcatheter was navigated through the basilar artery, left posterior communicating artery, left internal carotid artery, then through the area of injury into the cavernous sinus. Coils were placed in the cavernous sinus and back into the ICA. (C) Lateral view of left vertebral artery contrast injection after deployment of 3rd coil showing diminished CCF. Note the improved distal filling of the anterior cerebral circulation (arrow). (D) Lateral view of left vertebral artery contrast injection after 5th coil showing cure of CCF. The anterior cerebral circulation distal to the CCF continues to improve (arrow). (E) Unsubtracted lateral view of coil placement after treatment. (F) Follow up angiogram after treatment showing complete cure of CCF and improved distal filling of the anterior cerebral circulation (arrow). CCF, carotid-cavernous fistula; ICA, internal carotid artery
REFERENCES
1. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985 Feb;62(2):248-56.


2. Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: implications of a new grading scale. J Trauma. 1999 Nov;47(5):845-53.


3. Biffl CT, Nguyen D, Duc VT, Chau HH, Son VT. Direct traumatic carotid cavernous fistula: angiographic classification and treatment strategies. Study of 172 cases. Interv Neuroradiol. 2014 Jul-Aug;20(4):461-75.




4. Debrun GM, Ausman JI, Charbel FT, Aletich VA. Access to the cavernous sinus through the vertebral artery: technical case report. Neurosurgery. 1995 Jul;37(1):144-6; discussion 146.


5. Ellis JA, Goldstein H, Connolly ES, Meyers PM. Carotid-cavernous fistulas. Neurosurg Focus. 2012 May;32(5):E9.


6. Gemmete JJ, Ansari SA, Gandhi DM. Endovascular techniques for treatment of carotid-cavernous fistula. J Neuroophthalmol. 2009 Mar;29(1):62-71.


7. Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, Kizilkilic O. Endovascular treatment of carotid cavernous sinus fistula: A systematic review. World J Radiol. 2013 Apr 28 5(4):143-55.



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 288 View
- 9 Download
- ORCID iDs
-
Jonathan R. Crowe

https://orcid.org/0000-0003-3670-5566 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



