Management of a ruptured posterior inferior cerebellar artery (PICA) aneurysm with end-to-end in situ bypass: Case report
Article information
Abstract
Dissecting posterior inferior cerebellar artery (PICA) aneurysms are uncommon lesions. Their anatomy and the location of the dissection are variable, however, they usually occurs at the origin of the PICA. Dissecting PICA aneurysms generally have non-vascular morphology involving an entire segment of the artery and cannot be cut. Nevertheless, the detection of these vascular lesions has increased latterly, so it is necessary to recognize it and take the appropriate management modalities for these injuries. In this report, we describe a case of a 73-year-old male patient, who presented a history of severe headache, associated with neck stiffness, nausea, vomiting, dizziness, hypoactivity, mental confusion, and walking difficulty. Radiographic investigation with brain computed tomography (CT) showed mild bleeding in a pre-medullary and pre-pontine cistern, and cerebral angiogram showed a dissecting PICA aneurysm. Despite being a challenging treatment, microsurgery management was the chosen modality. It was performed an end-to-end anastomosis between the p2/p3 segments, showing to be effective with good clinical and radiographic outcomes. We discussed an unusual case, reviewing the current literature on clinical presentations, the angiographic characteristics of the dissecting aneurysms of PICA, and evaluating the clinical and angiographic results of patients undergoing microsurgical treatment.
INTRODUCTION
Dissecting posterior inferior cerebellar artery (PICA) aneurysm is very rare, representing only 0.5 to 0.7% of all intracranial aneurysms [12]. These aneurysms generally present hemorrhage or may show symptoms due to compression of the brainstem or lower cranial nerves [7,8]. Mortality from recurrent hemorrhage within 48 hours after the first rupture of PICA aneurysm is 3 times greater than that of aneurysms ruptured in the previous circulation. Despite this, the detection of these vascular injuries has increased in recent years. Therefore, it is necessary to recognize the diagnosis and the appropriate treatment modalities for these lesions [7,8].
Dissecting PICA aneurysm has non-saccular morphology, involving an entire segment of the artery. Such aneurysms are usually unclippable. Emergency treatment is vitally important in patients with ruptured PICA aneurysms. Exclusion of these ruptured aneurysms can be performed endovascularly or microsurgically by sacrificing the parent artery, or by revascularization of the PICA territory which is only achieved by the microsurgical technique [1,2,4,13].
There are several bypass techniques to perform revascularization of the PICA territory. This report shows the safety and efficiency of the microsurgical treatment of the dissecting PICA aneurysm through an end-to-end anastomosis in situ, despite its complexity.
CASE DESCRIPTION
JAS male patient, 73 years old, married, autonomous, hypertensive, and diabetic, denies smoking and drinking, he was admitted to the neurosurgical emergency at Hospital da Restauração on March 2020 with a history of sudden headache in the right paroccipital region of moderate-intensity, one week after admission. He sought for an emergency in the city of origin, was medicated, then he was discharged home due to an improvement in his condition and due to the COVID19 pandemic, he could not stay in the emergency any longer due to his age. Two days later, the cephalea worsened, with irradiation to the cervical region, associated with vomiting, and dizziness. It evolved with worsening dizziness, hypoactivity, mental confusion, and walking difficulty. Thus, he again sought medical service and in a diagnostic investigation in cranial computed tomography (CT) scan without contrast, bleeding was observed in a pre-pontine and pre-medullary cistern (Fig. 1).

Brain computed tomography scan without contrast, showing a subarachnoid hemorrhage in prepontine and premedullary cistern.
On admission, he was hemodynamically stable, conscious, confused, with Glasgow coma scale 14 (E4V4M6), presenting a stiff neck, without a focal deficit.
Performed cerebral angiography that showed a dissecting aneurysmal lesion in the anterolateral follow-up of the right PICA of regular contour, measuring about 4.3×2.9 mm in its largest dimensions (Fig. 2).

Cerebral angiogram, showing a dissecting aneurysmal lesion in the anterolateral segment of the right PICA. PICA, posterior inferior cerebellar artery
The patient underwent microsurgical treatment of the right dissecting PICA aneurysm, using the Far-Lateral approach. After opening the dura mater and the cisterna magna and slightly retracting the cerebellum inferolateral margin, the dissecting partially thrombosed aneurysm of PICA was evident, it was not amenable to conventional clipping, so the aneurysm was excluded through a direct cut between p2 (lateral medullary segment) and p3 (tonsilomedullary segment) for an end-to-end reconstruction. The main technical points for bypass in situ PICA-PICA include the extensive arachnoidal dissection to join the p2/p3 segments without tension; extraluminal suture with separate stitches. Thus, a termino-terminal anastomosis between the lateral medullary and tonsilomedullary was performed, using nylon10/0 thread with separate single stitches, 2 temporary clips (distal to p2 and proximal to p3), heparin, papaverine, and methylene blue. Firstly, before performing the anastomotic procedure, all arachnoid bands must be dissected to facilitate mobilization of the arteries. The most challenging point of the end-to-end anastomosis is the suture of the posterior suture line, the technique was performed with the aid of gentle rotation of the recipient and donor segments using microforceps and slight rotation in the microscope angle. The total clamp time was 32 min and 15 s. After the procedure, a revision was made and blood flow was tested with a vascular doppler pencil in the proximal and terminal portions of the PICA, with adequate flow through the anastomosis after the release of the temporary clips (Fig. 3). The total operation time was 5 h and 15 min.
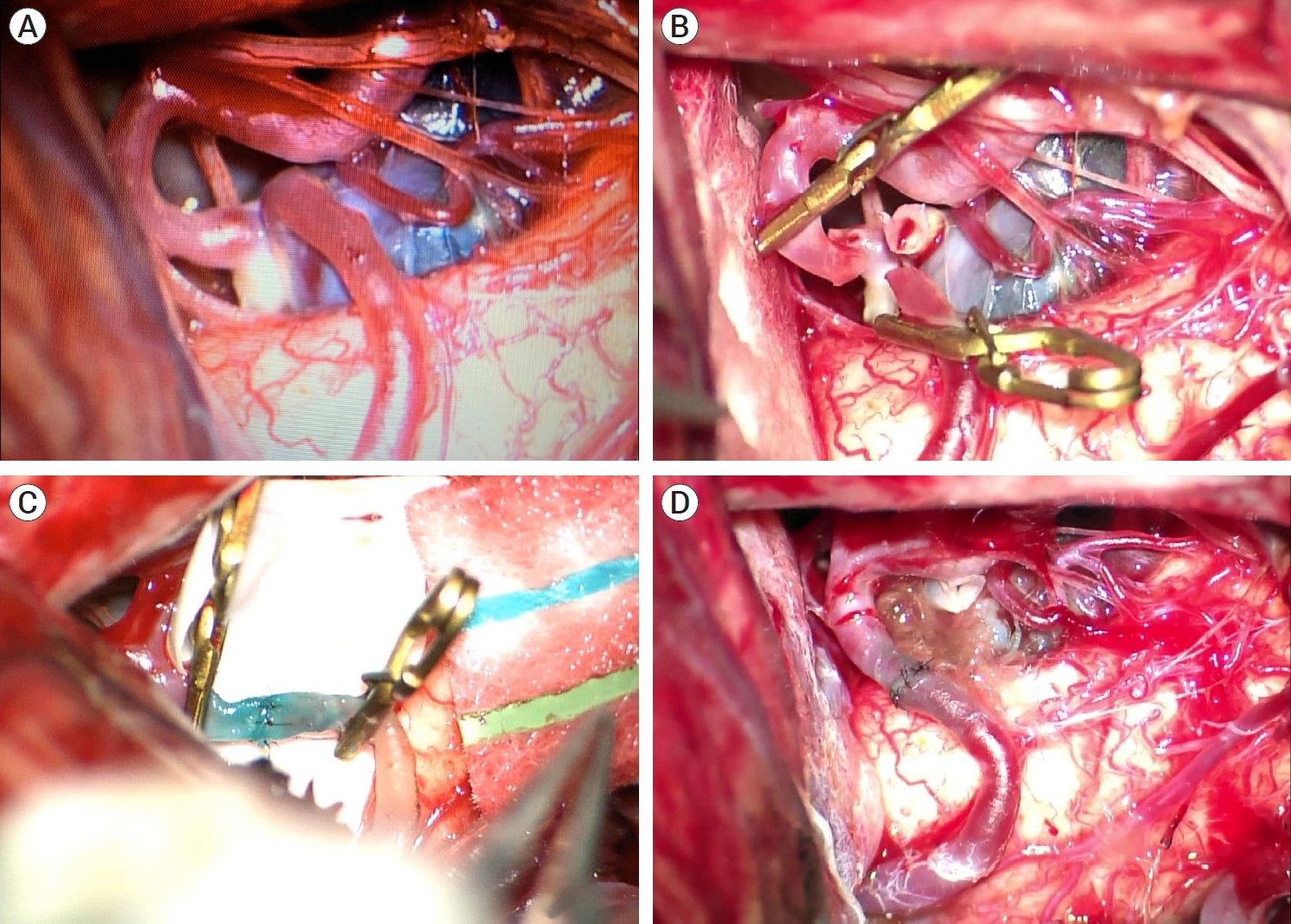
Far-Lateral approach was performed, under microscopy view, showing a dissecting partially thrombosed aneurysm of PICA (A). It was not amenable to conventional clipping, so the aneurysm was excluded through a direct cut between p2 (lateral bulbar segment) and p3 (tonsilobulbar segment) for an end-to-end reconstruction (B). A end-to-end anastomosis between the lateral bulbar and tonsilobulbar was performed, using nylon10/0 thread with separate single stitches, 2 temporary clips (distal to p2 and proximal to p3), heparin, papaverine, and methylene blue (C). Final aspect at the end of the procedure after the release of the temporary clips (D). PICA, posterior inferior cerebellar artery
The patient left stable and extubated in the operating room, we started Aspirin 300 mg in the immediate postoperative period, and blood pressure management. 24 hours after the procedure, the patient underwent control angiography, showing effective treatment of the dissecting aneurysm of PICA (Fig. 4). The patient remained clinically and neurologically stable, with no new complaints (Fig. 5).

Control cerebral angiogram, showing effective treatment of the dissecting PICA aneurysm. PICA, posterior inferior cerebellar artery
DISCUSSION
Posterior circulation aneurysms account for 10–15% of intracranial aneurysms. In these, the diagnosis is often secondary to subarachnoid hemorrhage. The international study of non-ruptured intracranial aneurysms (ISUIA) concluded that a posterior circulation aneurysm represents an independent risk factor for rupture in its natural history. PICA aneurysms are even more uncommon, accounting for 3-4% of all intracranial aneurysms and 20% of posterior circulation aneurysms [3,9]. Most injuries arise near the origin of PICA from the vertebral artery (VA). Besides, PICA aneurysms are often located distally in the artery, rather than appearing at branch sites in the artery, which differs significantly from aneurysms elsewhere [9]. These aneurysms are also classified as saccular and fusiform. Saccular lesions are hemodynamically generated lesions that usually appear in bifurcations or curves of the vessels and can be treated surgically or endovascularly without sacrificing the parent vessel. Fusiform aneurysms appear spontaneously anywhere in the course of the vessel as a result of dissection [13].
Dissecting aneurysms of the PICA are very rare, present a high risk of bleeding, and are generally not amenable for clipping. Exclusion of these ruptured aneurysms can be performed by endovascular or microsurgical route, sacrificing the affected artery, or by revascularization of the PICA territory, which is only achieved by the microsurgical technique [2,4,5,11,13].
Microsurgical treatment of posterior circulation aneurysms is complex and challenging for neurosurgeons due to the particular anatomy of the region, depth of surgical approach, and an intimate relationship with the brainstem and cranial nerves [5,11]. There are several bypass techniques, to perform the revascularization of the PICA territory. There is an extracranial-intracranial bypass (EC-IC) and intracranial-intracranial bypass (IC-IC). EC-IC bypass is revascularization using scalp arteries from the external carotid arteries as donors to reconstruct the flow of intracranial arteries [10]. In the presented case, the occipital artery was prepared to perform a possible EC-IC bypass, however, during the intraoperative period, an IC-IC bypass was chosen.
Bypass IC-IC is used preferably when revascularization is required to manage complex aneurysms. PICA aneurysms have a better application of the IC-IC bypass than any other aneurysms. This fact occurs due to the proximity of the two PICAs and their branches, allowing several possibilities for IC-IC bypass [1,2,13].
The selection of the PICA bypass depends on the location of the dissecting aneurysm along with the segments. For aneurysms trapped at the origin of the PICA or p1 segment (anterior medullary segment), as an alternative to revascularization, there is the laterolateral bypass of the two PICAs or PICA reimplantation in the VA as an alternative. For aneurysms of the p2 segment (lateral medullary segment) as an alternative to revascularization in addition to PICA reimplantation and PICA latero-lateral bypass, there is in situ bypass, bypassing the aneurysm. For distal aneurysms of the p3 segment (tonsilomedullary segment) as an alternative for revascularization, there is the PICA in situ bypass and PICA laterolateral bypass. And for aneurysms of the p4 segment (telovelotonsillar segment) that are very distal to the PICA-PICA laterolateral deviation, they are resuscitated in situ [1].
In the case reported, as it is a PICA-p3 segment PICA dissecting aneurysm, we opted for reanastomosis through in situ bypass to bypass the aneurysm. In cases with dominant PICA, it is preferable to avoid reanastomosis through the altero-lateral bypass of the two PICAs, due to the risk of compromising the dominant PICA and risk of ischemia in case the anastomosis is not satisfactory due to bypass occlusion or prolonged temporary clipping [1,2,13].
Therefore, the PICA-PICA laterolateral bypass can be used for PICA aneurysms in any segment, except p4. In situ reanastomosis can be used with PICA aneurysms after the p1 segment. Graft interposition is rarely used for reanastomosis in the management of PICA aneurysm [1,6].
Currently, endovascular techniques are used more frequently and few surgeons feel comfortable performing microsurgical bypass techniques. Thus, it is common for patients like the one in the reported case to undergo endovascular procedures that sacrifice PICA. Despite this, the clinical effects of ischemia resulting from PICA occlusion are variable and can be quite disabling if the patient has a dominant PICA or if there is an occlusion in a location close to the perforating brainstem. Therefore, a constructive approach that preserves the PICA with a reconstruction of the flow by a bypass should be the first alternative considered when the complete occlusion of the aneurysm is unlikely [1,2].
CONCLUSIONS
Therefore, the safety and efficiency of the microsurgical treatment of dissecting PICA aneurysm are noted, despite its complexity. According to the literature reviews, the microsurgical procedure, when properly indicated and performed, presents satisfactory results both from a clinical and radiological point of view.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.

