 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 25(4); 2023 > Article |
|
Abstract
Thrombectomy procedures following intra-aneurysmatic lesions are extremely rare, and few cases have been reported. This article describes a microsurgical intra-aneurysmatic thrombectomy (MIaT) for a distal anterior cerebral artery (DACA) aneurysm. We present the case of a 48-year-old female that was admitted to the emergency room, showing neurologic deterioration with focal deficits. A computed tomography angiography (CTA) scan revealed an aneurysm located in the distal segment of the left anterior cerebral artery. During the surgical procedure, after clipping, a wellformed clot was visualized through the aneurysmãs wall obstructing the left DACA flow. We proceeded to open the aneurysmãs dome to remove the thrombus and clip the aneurysm neck, re-establishing the flow of the left DACA.
Intra-aneurysmatic thrombosis can occur as a complication during clipping, obstructing the distal flow of vital arteries and causing fatal results in the patientãs postoperative status. MIaT is a good technique for restoring the flow of the affected vessel and allows a secure aneurysm clipping after thrombus removal.
DACA aneurysms are relatively rare, representing about 6% of all intracranial aneurysms. These are located between the A2 and A5 segments of the anterior cerebral artery [8]. Intraoperative complications may occur, being aneurysmatic rupture the most frequent, causing bleeding and localized vasospasm with infarction of a vascular territory [9,13]. However, the formation of a thrombus inside the aneurysm as a complication during microsurgical or endovascular procedures is rare, and few descriptions have been found in the literature [1,2,5]. Microsurgical thrombectomy has been well described as a treatment for cerebral ischemic disease affecting the M1 segment or the bifurcation of the middle cerebral artery. We present an illustrative case of a distal anterior cerebral artery (DACA) thrombosis as a complication during aneurysm clipping, being resolved with microsurgical intra-aneurysmatic thrombectomy (MIaT), restoring the distal artery flow, and achieving a complete occlusion of the aneurysmãs neck.
We describe the case of a 48-year-old female with a previous history of hypertension who was admitted to our emergency room due to generalized seizures. Neurological examination revealed a Glasgow coma scale of 11 (E3, V2, M6), a right central facial palsy, and a 3/5 right hemiparesis. A CT scan revealed a Fisher IV subarachnoid hemorrhage, an aneurysmatic lesion in the left DACA, and an associated right frontal intraparenchymal hematoma. Computed tomography angiography (CTA) and 3D reconstructions were performed to visualize the aneurysmãs dome projection and identify the related arteries (Fig. 1).
A surgical procedure was deemed necessary following the clinical condition and imaging findings. During surgery, the patient was supine with the head fixed on a Mayfield-Kees head holder in a neutral position. A bifrontal craniotomy with a conventional anterior interhemispheric approach was performed. Under the microscopic vision, cerebrospinal fluid was depleted while opening the interhemispheric fissure. To improve the surgical vision, we removed the right frontal and interhemispheric hematoma, identifying both A2 arteries and using a temporary clip in the left A2 artery to achieve aneurysm dome dissection. The aneurysm was attached to the callosomarginal branches and was thoroughly dissected with microsurgical techniques, identifying the neck and the distal segment of the left anterior cerebral artery. A 7 mm straight clip (Aesculap, PA, USA) was applied to the aneurysmãs neck. Posteriorly, the patency of the left A3 segment was verified with intravenous fluorescein, and no flow was observed through this artery (Fig. 2). An intra-aneurysmatic thrombus was observed through the aneurysm wall, explaining the flow obstruction. We decided to place a proximal temporary clip in the left A2 segment, and the aneurysm dome was opened linearly using a microscissor, corroborating the formation of an intra-aneurysmatic thrombus as a complication after clipping. The thrombus was located inside the aneurysm and a partly extended towards the DACAãs lumen. MIaT was performed using continued saline solution irrigation for the thrombus dissolution and microdissectors and microforceps to separate the thrombus from the vessel wall following a circumferential dissection (Figs. 3 and 4). We identified a small rupture on the aneurysmãs neck, where we put a 3 mm straight miniclip (Aesculap, PA, USA). The previous 7 mm straight clip was repositioned on the aneurysmãs neck, achieving a complete occlusion of the aneurysm. Once again, the patency of the left A3 segment was verified using intravenous fluorescein. Craniectomy in this patient was deemed necessary due to brain edema. A postoperative CTA scan was performed for adequate corroborating flow in both DACAs (Fig. 5). During the postoperative course, the patientãs consciousness and left hemiparesis improved 4/5 with sequel right central facial palsy. Follow-up was performed during the first month and posteriorly every three months at clinics.
After a thorough literature review, we found some case reports where performing an intra-aneurysmatic thrombectomy was feasible [3,7,10,12]. Hirano et al., reported a case of an emergent thrombectomy in an anterior communicating artery aneurysm [5]. In this case, the decision to perform a MIaT was evidence of a thrombus inside the aneurysm during the procedure, obstructing the left DACA flow, corroborated with intravenous fluorescence.
In this case, we could consider leaving the aneurysm clipped and opening the left DACA with a small linear incision to remove the thrombus, followed by primary closure using simple stitches with 10-0 sutures. However, the risk of lumen stenosis is high, and it might not be possible to reach the intra-aneurysmatic component and leave a residual portion. Although surgical thrombectomy has been described in occlusion of large cerebral vessels [6], mainly in cerebral ischemic disease, microsurgical thrombectomy is an adequate tool that can be mastered by the neurosurgeon and employed when a complication occurs in the setting of surgical clipping.
In this case, restoring the flow was imperative to avoid postoperative complications. Endovascular therapy could be considered to remove the thrombus as it now permits simultaneously treating aneurysmal and occlusive vascular pathology [1,2,4,11]. Unfortunately, it was not available in our operating room, and transferring the patient to the endovascular suite could pose a severe risk for ischemic complications. Open thrombectomy continues to be a valuable tool for acute treatment of large vessel occlusion when endovascular therapy is not possible, reporting a recanalization rate of up to 96.2% with clinical improvement in about half of the patients; however, MIaT must be carefully performed in individualized cases and by senior surgeons, taking in count that the aneurysm wall does not share the same structure as a normal vessel (for example in large vessel occlusion). Therefore its manipulation can cause damage to the neck affecting the recovery process of the vessel after clipping [6]. More studies are required to determine the safeness and effectiveness of this complication management.
We attribute the development of the thrombus due to the manipulation during aneurysmal dissection. Although there is scarce evidence about this microsurgical alternative, we can consider using the MIaT when a similar complication occurs.
MIaT is a procedure that has yet to be well described in the literature during aneurysm clipping. It is essential to verify the patency of the distal branches after clipping the aneurysm to transoperatively identify this complication, which, although rare, can cause a change in the patientãs prognosis. Vascular anatomical knowledge is essential during this type of procedure.
Fig.ô 1.
(A) Axial CTA showing a saccular aneurysm in the distal anterior cerebral artery. (B) 3D-reconstruction of the coronal CTA with evidence of a saccular aneurysm with a superior dome projection between callosomarginal and pericallosal arteries. CTA, computed tomography angiography

Fig.ô 2.
(A) Intraoperative images showing the DACA aneurysm clipping with a 7 mm straight clip. (B) Patency of the left pericallosal artery was verified with intravenous fluorescein and no flow was observed. DACA, distal anterior cerebral artery
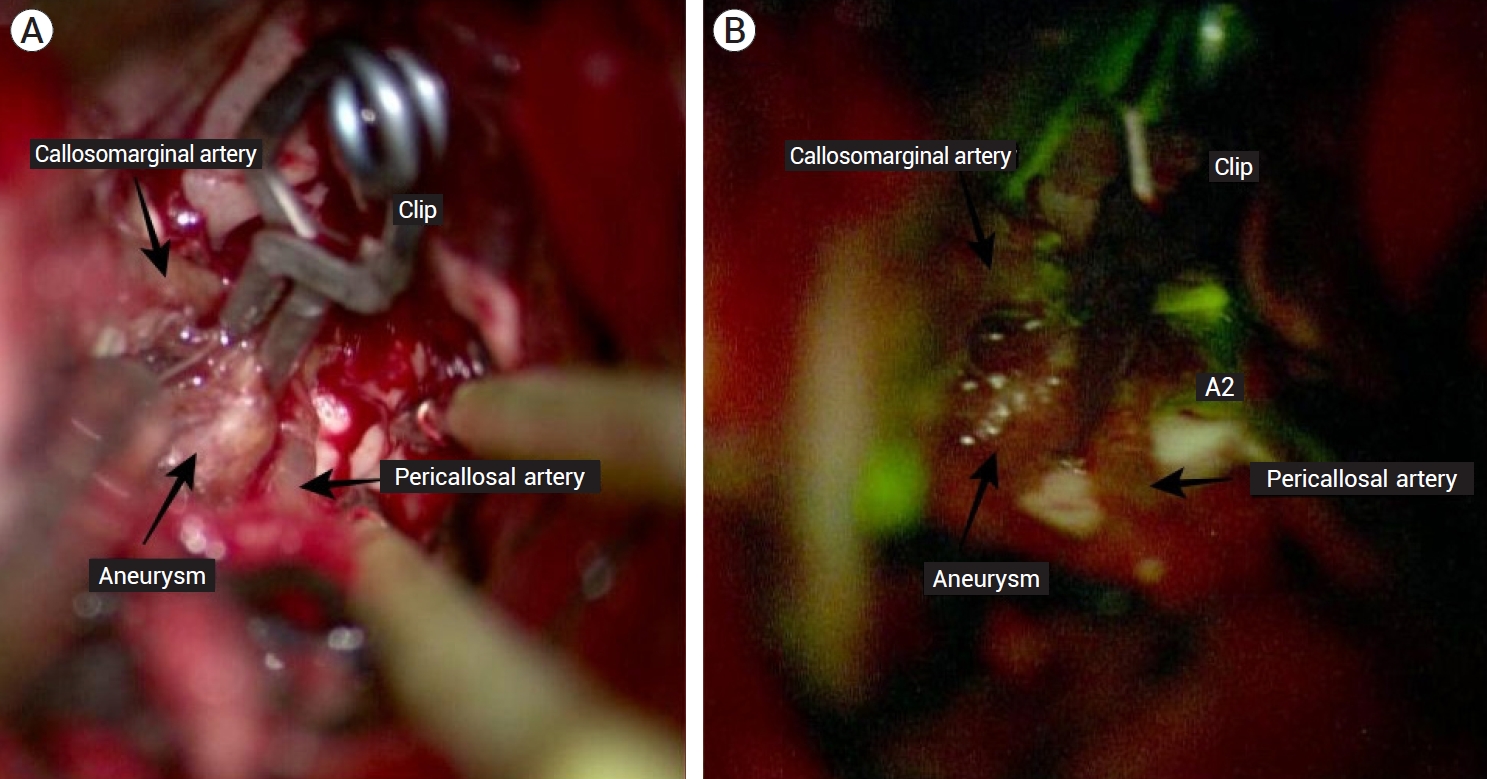
Fig.ô 3.
Artist ilustration showing the steps of microsurgical intra-aneurysmatic thrombectomy. (A) First, the aneurysm dome was opened using microscissors. (B) Microdissector was used to dissect the intra-aneurysmatic clot and remove it. (C) Irrigation using saline solution was employed in order to achieve the artery patency. (D) Final clipping with a 3 mm straight miniclip for the neck rupture and a 7 mm straight clip for complete aneurysm occlusion.

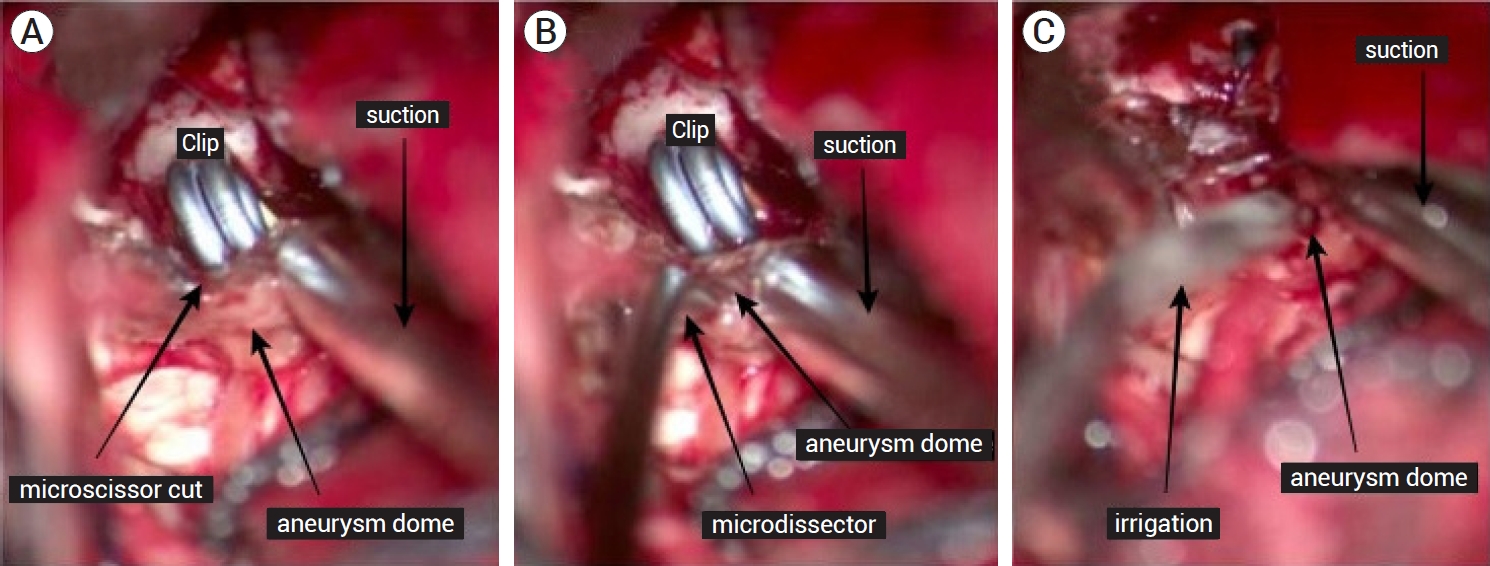
Fig.ô 4.
Intraoperative illustrations. (A) Aneurysmãs dome was already cut with microscissors. (B) Microdissector was introduced in the aneurysmãs dome to dissect the intra-aneurysmatic clot. (C) Irrigation with saline solution was used inside the aneurysm to remove the clot and achieve the arterial patency.
REFERENCES
1. Ahn JH, Jun HS, Song JH, Cho BM, Lee HK, Kim BC, et al. Rescue mechanical thrombectomy using a retrievable stent for thromboembolic occlusion occurring during coil embolization of ruptured intracranial aneurysms. J Neurointerv Surg. 2017 Mar;9(3):244-9.


2. Briganti F, Leone G, Marseglia M, Chiaramonte C, Solari D, Caranci F, et al. Mechanical thrombectomy in the treatment of distal occlusions during coil embolization of ruptured intracranial aneurysms. NMC Case Rep J. 2016 Sep;3(4):115-7.



3. Harada K, Kurokawa T, Kato S, Ishihara H, Saka M, Oka F, et al. Operative open intra-aneurysmal thrombectomy for ruptured cerebral aneurysm and peripheral ischemia associated with vasospasm. J Clin Neurosci. 2010 Apr;17(4):517-20.


4. Hirata K, Yamazaki T, Kato N, Yasuda S, Matsumura A. Mechanical thrombectomy for occlusion near a ruptured intracranial aneurysm: A case report. Surg Neurol Int. 2020 May;11:120.



5. Hirano Y, Ono H, Inoue T, Mitani T, Tanishima T, Tamura A, et al. Emergent surgical embolectomy for middle cerebral artery occlusion related to cerebral angiography followed by neck clipping for an unruptured aneurysm in the anterior communicating artery. Surg Neurol Int. 2020 Dec;11:420.



6. Horiuchi T, Nitta J, Miyaoka Y, Nagm A, Tsutsumi K, Ito K, et al. Open embolectomy of large vessel occlusion in the endovascular era: Results of a 12-year single-center experience. World Neurosurg. 2017 Jun;102:65-71.


7. KheáÙreddin AS, Filatov IuM. Microsurgical treatment of partially thrombosed giant cerebral aneurysms--technique of endoaneurysmal thrombectomy. Zh Vopr Neirokhir Im N N Burdenko. (Russian). 2008 Oct-Dec;(4):49-51; discussion 51.
8. Lehecka M, Dashti R, Lehto H, Kivisaari R, NiemelûÊ M, Hernesniemi J. Distal anterior cerebral artery aneurysms. Acta Neurochir Suppl. 2010 107:15-26.


9. Pfaff J, Herweh C, Pham M, Schieber S, Ringleb PA, Bendszus M, et al. Mechanical thrombectomy of distal occlusions in the anterior cerebral artery: Recanalization rates, periprocedural complications, and clinical outcome. AJNR Am J Neuroradiol. 2016 Apr;37(4):673-8.



10. Sugita M, Kinouchi H, Nishiyama Y, Kanemaru K, Yoshioka H, Horikoshi T. Direct clipping of a thrombosed giant cerebral aneurysm after thrombectomy without bleeding to minimize the temporary occlusion time: Technical case report. Neurol Med Chir (Tokyo). 2009 Dec;49(12):600-3.


11. Singh J, Wolfe SQ. Stent retriever thrombectomy with aneurysm in target vessel: Technical note. Interv Neuroradiol. 2016 Oct;22(5):544-7.




- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 844 View
- 16 Download
- ORCID iDs
-
Ricardo Marian-MagaûÝa

https://orcid.org/0000-0002-0518-9629 - Related articles
-
Microsurgical Anatomy of the Anterior Cerebral Artery.2000 September;2(2)
Kissing Aneurysms of Distal Anterior Cerebral Arteries: A Case Report.2001 March;3(1)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



