 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 26(1); 2024 > Article |
|
Abstract
Objective
To review the characteristics of distal middle cerebral artery (MCA) aneurysm treated by microsurgery, the detailed surgical options, and the clinical result.
Methods
We retrospectively reviewed cerebral aneurysm in the M2 and M3 segments of the MCA surgically treated between January 2015 and December 2022. The demographic data, aneurysm-related findings, type of surgical approach, surgical technique, and clinical outcomes of the enrolled patients were analyzed.
Results
Sixteen distal MCA aneurysms were treated with microneurosurgery (incidence, 1.0%; female, 12; mean age, 58.1 years; ruptured, three). Twelve aneurysms were in the M2 segment (insular segment), two aneurysms at the M2-M3 junction, and two aneurysms in the M3 segment (opercular segment). Twelve aneurysms were saccular (average size, 4.9 mm; multiplicity, 50%; average aneurysms, 3.0; partially thrombosed, 1; sidewall aneurysm, 2). Three aneurysms were fusiform, of which two were ruptured. Of the ruptured aneurysms, one was a ruptured dissecting aneurysm. The trans-sylvian and trans-sulcal approaches were used in fourteen and two patients, respectively. Neck clipping, wrap clipping, and surgical trapping were performed in twelve, one, and one patient, respectively. Proximal occlusion was performed in one patient. Bypass technique was required in two patients (neck clipping and proximal occlusion). The modified Rankin Score was 6 in the two patients with ruptured aneurysms. The remaining patients did not show further neurological deterioration after microneurosurgery.
Distal middle cerebral artery (MCA) aneurysms can be described as aneurysms of the M2 segment (insular segment), M2-M3 junction, M3 segment (opercular segment), and M4 segment (cortical segment) according to the Gibo classification [6]. Distal MCA aneurysms are rare and have distinct features compared to the most common MCA aneurysms located at the M1-M2 junction or MCA bifurcation. Distal MCA aneurysms have a higher percentage of being fusiform or dissecting aneurysms and are usually related to trauma and cardiovascular infections [10,16].
Distal MCA aneurysms have low incidence, are usually deep-seated in the distal part of the sylvian cistern, covered with irregularly formed sylvian veins, and frequently have a nonsaccular shape. Consequently, its anatomy is unfamiliar, and the surgical approach and occlusion of the aneurysm may be difficult [5].
Owing to its rarity, the anatomy of a distal MCA aneurysms is often unfamiliar to surgeons. Because of its distant location, narrow lumen and association of anatomical variations it is prone to complications and difficult to access endovascularly. Because of its shape, which may be presented as a fusiform or dissecting type aneurysm it is often difficult to embolize the aneurysm itself. Thus, surgery is usually considered the first treatment option [5,21,22,24]. However, its anatomical position and high incidence rate of being a fusiform aneurysm still pose a large obstacle to the surgeon. Hence, in this study, we reviewed the characteristics of distal MCA aneurysms treated with microsurgery, surgical options, and clinical results.
This study was approved by the Institutional Review Board (IRB No. 2023-05-054). We retrospectively reviewed a list of cerebral aneurysm treatments performed at a single high-volume tertiary hospital. We investigated cerebral aneurysm cases surgically treated between January 2015 and December 2022. During the same period, we reviewed a list of cerebral aneurysms treated with endovascular procedures.
Patients who underwent surgical treatment for cerebral aneurysms located in the M2 and M3 segments of the MCA according to the Gibo classification were included [6]. Patients with other vascular diseases (Moyamoya disease, arteriovenous malformation, dural arteriovenous fistula, symptomatic atherosclerosis, etc.) that may have affected the incidence rate of cerebral aneurysms and aneurysms that seemed to be in the insular segment but were anatomically considered as MCA bifurcation aneurysms were excluded.
The demographic data, underlying disease, aneurysm location, morphology, size, other aneurysms, Hunt-Hess grade, modified Fisher grade, pre-/post-treatment modified Rankin Scale (mRS), type of surgical approach, surgical technique, and use of the surgical navigation system were analyzed for the enrolled patients.
The morphology of the cerebral aneurysm was classified as saccular, fusiform, dissecting, traumatic, or infectious, according to the International Study of Unruptured Intracranial Aneurysms [27].
Surgeries were performed under general anesthesia. All routine operations were performed using intraoperative neuromonitoring (NIM-Eclipse; Medtronic, FL, USA). A surgical navigation system (Curve® Navigation, Brainlab, Germany) was used when necessary. The trans-sylvian approach involves Sylvian fissure dissection, followed by access to the aneurysm. The trans-sulcal approach involves opening the sulcus starting from the distal branch of the distal MCA aneurysm. Surgical techniques for the treatment of cerebral aneurysms can be classified as neck clipping, wrap clipping, proximal occlusion, trapping, and additional bypass, if necessary. The use of a surgical navigation system during the procedure can also be considered as a separate category.
Between January 2015 and December 2022, clipping was performed on 1556 aneurysms in our institute. Of these, 807 were MCA aneurysms. MCA aneurysms had an average age at diagnosis of 60.3 years. There were 576 MCA aneurysms in women and 231 in men. 167 MCA aneurysms were treated in ruptured condition. Among the aneurysms treated with clipping, 16 were confirmed to be distal MCA aneurysms, as previously defined (incidence, 1.0%). During the same period, endovascular treatment was performed for 1678 aneurysms, of which 135 were MCA aneurysms and 4 were distal MCA aneurysms. The average age at diagnosis of distal MCA aneurysms were 58.1 years. The patients included 12 women and 4 men. Four patients received treatment during the acute phase of subarachnoid hemorrhage (SAH). SAH due to a distal MCA aneurysm was observed in three patients. One patient had an SAH due to the rupture of another aneurysm. One of these cases was converted to endovascular treatment during surgery (Table 1).
Twelve aneurysms were located in the M2 segment (insular segment), two at the M2-M3 junction, and two in the M3 segment (opercular segment). Regarding the morphology of the cerebral aneurysms, 12 were saccular, all of which were nonruptured. Among these, one had partial thrombosis and two were sidewall aneurysms. The average size of the saccular aneurysm was 4.9 mm (range, 1.6-14 mm). Three of the aneurysms were of the fusiform type and two of these had ruptured. There was no evidence of infection or trauma. The mean length of the fusiform aneurysms was 8.7 mm. One patient had a 15-mm-long dissecting aneurysm. Multiple aneurysms were only observed in patients with saccular aneurysms. Six patients had multiple cerebral aneurysms, with an average of three aneurysms per person (Table 2).
Surgery was performed in 14 patients using the trans-sylvian approach. Surgical navigation was used in one of these cases. Case 9 was of a ruptured aneurysm. Because of severe brain edema during surgery, the aneurysm could not be accessed, and the surgery was aborted and converted to endovascular treatment. Eventually, it was trapped using an endovascular coil. Case 10 had a fusiform aneurysm approximately 11 mm in length in the M3 segment. The trans-sylvian approach was performed using the surgical navigation system. The inlet was occluded with multiple clips, and the normal distal branches passing through the outlet of the aneurysm were anastomosed with the parietal branch of the superficial temporal artery (STA) (Fig. 1). Case 12 involved a dissecting aneurysm in the M2 segment. Wrap clipping was performed using a bemsheet and 3 clips (Fig. 2). Case 15 had a ruptured fusiform aneurysm and trapping was performed using two clips.
In two patients, surgery was performed using a transsulcal approach guided by the surgical navigation system. Case 7 had a partially thrombosed saccular aneurysm at the M2-M3 junction. First, the neck of the aneurysm was clipped. However, distal blood flow in one branch was weakened, and a signal change was detected on intraoperative neuromonitoring. Therefore, anastomosis using the parietal branch of the STA was performed (Fig. 3). Neck clipping was performed in another patient.
The mRS score eventually reached 6 in the two patients who had ruptured aneurysms. The other patients did not show further neurological deterioration owing to microneurosurgery. The mRS was 0 in 13 patients, and 4 in one patient, which was because of the rupture of another aneurysm.
Distal MCA aneurysms are rare and have an incidence of 1-5% according to previous reports [5,8,11,17]. In our retrospective study, the incidence (of 16 distal MCA aneurysm cases treated with microneurosurgery) was approximately 1%. Furthermore, when patients who underwent endovascular treatment were included, this value decreased to 0.59%. The reason for the low number of patients in this study may be that only treated cerebral aneurysms were surveyed.
Distal MCA aneurysms have a higher incidence of nonsaccular or fusiform aneurysm [4,11]. In our study, 25% (4 out of 16) of the patients had nonsaccular aneurysms. In general, the incidence of fusiform intracranial aneurysms is 3-13% [19]. Our study showed relatively high rate of fusiform aneurysms at 18.8% (3 out of 16). However, because of its low incidence, the rate at each institute may vary. Among the three ruptured distal MCA aneurysms, two were of the fusiform type (including dissecting aneurysms), which supports the notion that distal MCA aneurysms of the fusiform type are more likely to rupture.
Distal MCA aneurysms are often accompanied by multiple aneurysms. The incidence of having an additional aneurysm is approximately 50% [4,5,8]. However, these results were based on very small samples. In our study, six patients (38%) had multiple aneurysms. Considering saccular aneurysms, the rate was 50%, with an average of three aneurysms. Interestingly, none of the distal saccular MCA aneurysms ruptured. Furthermore, although there were just four patients, multiple cerebral aneurysms were not found in patients with nonsaccular cerebral aneurysms and three out of the four nonsaccular aneurysms ruptured.
Trauma and mycotic emboli have also been reported to cause distal MCA aneurysms [3,7,11,25]. However, these causes were not identified in the present study. Mycotic aneurysms frequently occur in the distal MCA region. Mycotic aneurysms are extremely rare and their incidence is declining. Even if an intracerebral hemorrhage is diagnosed, cerebral aneurysms are often underdiagnosed on computed tomography angiography or magnetic resonance angiography [20]. During the study period, a few cases of mycotic aneurysms were detected that did not require surgery and were not included in the study.
We classified the location of the aneurysms into three types using the Gibo classification [6]. Of the 16 cases, 12 involved the M2 segment, 2 were at the M2-M3 junction, and 2 cases involved the M3 segment. The incidence of distal MCA aneurysms was higher in the M2 segment than elsewhere, corroborating with the results of previous studies [4,8,11,22].
Owing to these characteristics of distal MCA aneurysms, wide dissection of the Sylvian cistern is necessary. However, the anatomy of the Sylvian veins has variations [9]. Different techniques and approaches for dissecting Sylvian veins should be considered to minimize complications of venous injury [14]. However, it may be impossible to reach the M2-M3 junction or M3 segment lesions using the trans-sylvian approach. In such cases, the trans-sulcal approach may be useful [5]. We treated two cases using the trans-sulcal approach, and both cases were well treated. We used the surgical navigation system three times, including in two cases involving trans-sulcal approaches. This was helpful in maintaining the right path to the target aneurysm [13,26].
The simplest method to treat a cerebral aneurysm is to excise the aneurysm from the bloodstream. A saccular aneurysm can be treated relatively simply using an aneurysm clip. However, this may not be straightforward for nonsaccular aneurysms. Distal MCA aneurysms may have a higher rate of being fusiform [11,15]. Fusiform aneurysms and dissecting aneurysms should be treated differently from typical nonsaccular aneurysms using techniques like wrapping, wrap clipping, trapping, or parent artery occlusion with bypass if needed [1,2,5,11,12,18,23]. Patients who underwent trapping or parent artery occlusion with bypass, infield Indocyanine green angiography played a significant role in determining the patency of the remaining vessels and anastomosis site after excluding aneurysms. Such evaluation helped limit post-operative neurologic deficits [1,18].
In this study, we encountered one case of ruptured dissecting aneurysm with a length of 15 mm, which was treated using the wrap clipping technique with bemsheet and 3 clips. The patient was stable, and the aneurysm did not recur. Furthermore, we experienced two unruptured aneurysm cases that required the vascular bypass technique. One was an M3 fusiform type aneurysm, in which we performed proximal occlusion and STA-MCA bypass, and the other was at the M2-M3 junction, where the arterial flow diminished after clipping the neck of the saccular aneurysm, followed by STA-MCA anastomosis. No patient had post-operative neurological deficits. Because distal MCA aneurysms may not be easily accessible, we also found proximal occlusion with vascular bypass to be a viable option [1,13].
Our study has some limitation as it used a retrospective design and data from surgically treated cerebral aneurysms, including a small sample of distal MCA aneurysms. Hence, further studies are necessary to determine the appropriate management of distal MCA aneurysms.
Distal MCA aneurysms had a high incidence of being diagnosed with multiple other aneurysms and were relatively nonsaccular in this series. Microneurosurgery of distal MCA aneurysms is challenging. Careful planning of the surgery in advance, appropriate use of a surgery-assisting device, and application of the vascular bypass technique were helpful in improving the treatment outcome.
Fig. 1.
Intraoperative field view of Case 10. (A) Fusiform aneurysm and afferent and efferent arteries can be identified through the wide sylvian dissection. Asterix indicates the fusiform aneurysm. The black arrow indicates an afferent artery of the aneurysm, and white arrow indicates the efferent arteries. (B) Temporary occlusion of the afferent artery (white arrow indicates a temporary clip in the afferent artery). (C) The connected afferent artery and one efferent artery close to the afferent artery, and the occluded trunk of the aneurysm with three clips. The white arrow indicates the anastomosis site of the other efferent artery with the parietal branch of the superficial temporal artery. (D) Indocyanine green angiography shows well preserved two efferent arteries (the yellow arrow indicates the blood flow from afferent artery to efferent artery, and the white arrow indicates the patent anastomosis site).
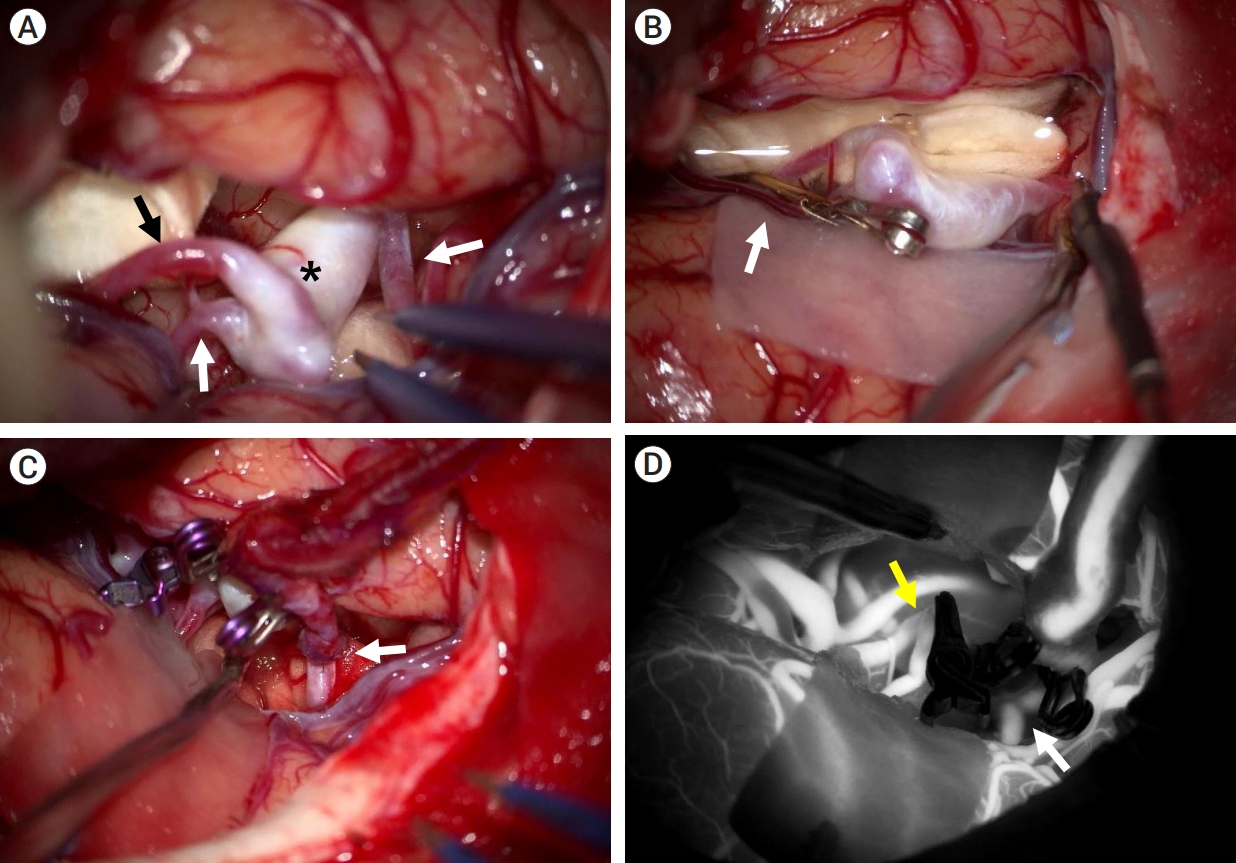
Fig. 2.
Intraoperative field view of Case 12. (A) An approximately 15-mm-long dissecting aneurysm is identified after performing wide dissection of the sylvian cistern. The white arrow indicates the endpoint of the dissection. (B) Wrap clipping performed using bemsheet and three clips.
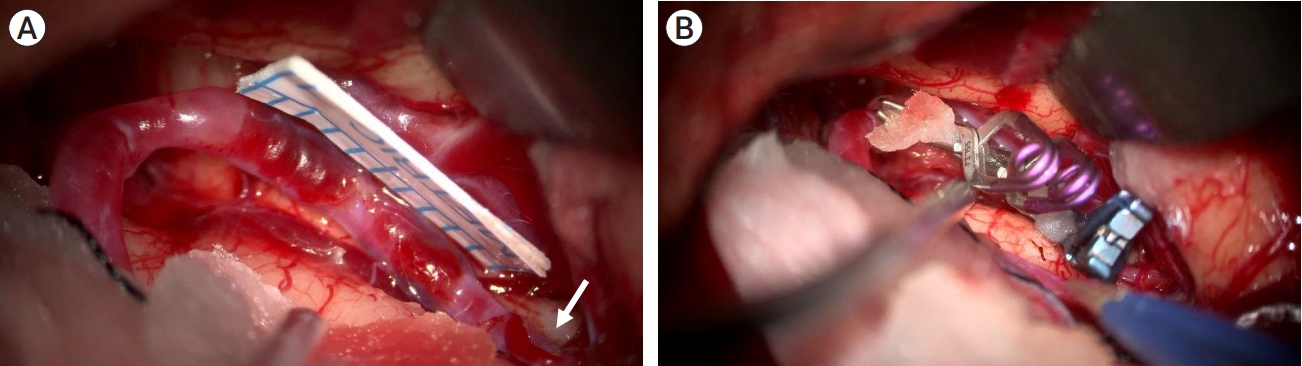
Fig. 3.
Three-dimensional rotation angiography image and intraoperative field view of Case 12. Thrombosed large aneurysm in distal middle cerebral artery. (A) Three-dimensional rotation angiography image reveals non-thrombosed part of the aneurysm. (B) Indocyanine green angiography shows lack of blood flow in one branch after neck clipping (white arrow). (C) Computed tomography angiography after clipping reveals patency of the occluded branch. (D) Occluded distal branch anastomosed with the parietal branch of the superficial temporal artery. The white arrow indicates the anastomosis site.
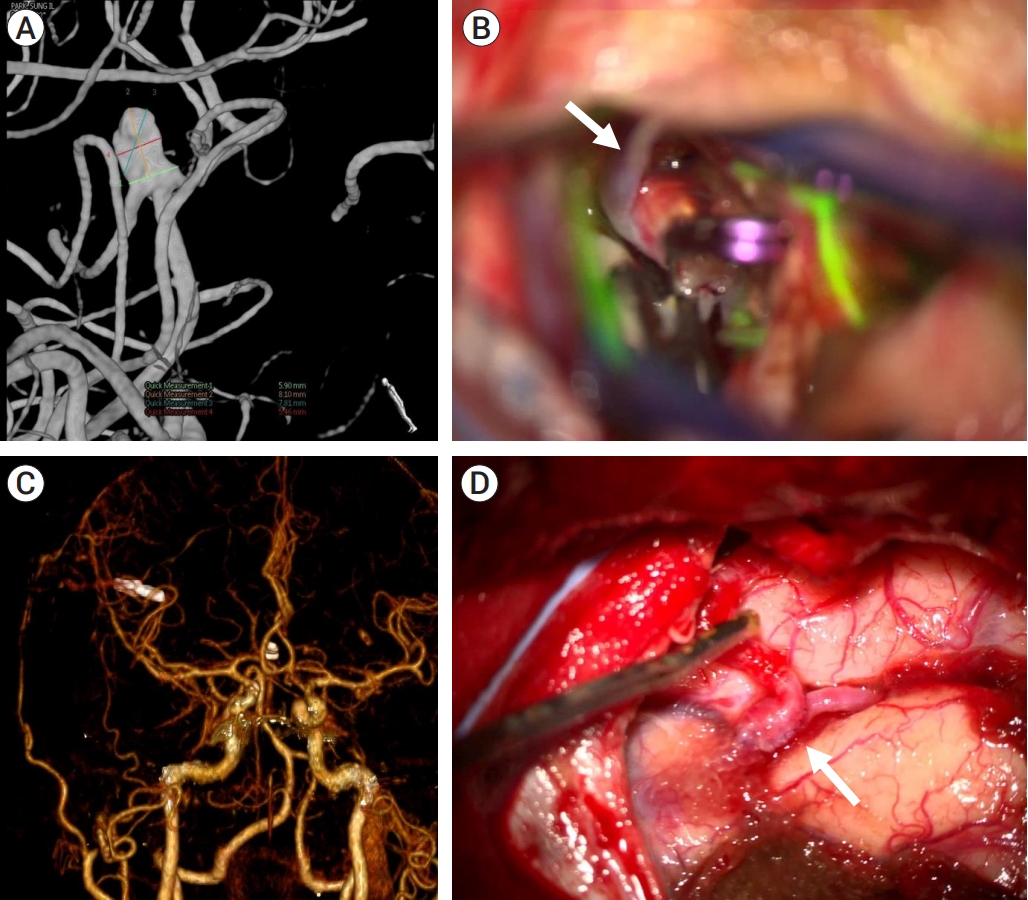
Table 1.
Demographics of MCA and distal MCA brain aneurysms treated from 2015 to 2022
| Total=3234 (aneurysms) | MCA | Distal MCA | MCA | Distal MCA | |
|---|---|---|---|---|---|
| Microsurgical treatment=1556 | 807 | 16 | Age (year) | 60.8 | 58.1 |
| M : F | 231:576 | 4:12 | |||
| Unruptured | 640 | 8 | |||
| Ruptured | 167 | 4 | |||
| Endovascular treatment=1678 | 135 | 4* |
Table 2.
Characteristics, surgical type, and treatment results of the microsurgical cases of distal middle cerebral artery aneurysm
| No. | Sex | Age | Location | Initial HHG | mFG | Shape | Anatomical morphology | Size (mm) | Multiple AN | Number of AN | Approach | Surgical navigation | OP result 1 | OP result 2 | mRS pre | mRS post |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 63 | Rt. M2 UR | 0 | Saccular | Bifurcation | 6.8 | Y | 3 | Trans-sylvian | Neck clipping | 0 | 0 | |||
| 2 | F | 44 | Rt. M2-M3 junction UR | 0 | Saccular | Bifurcation | 2.4 | Y | 2 | Trans-sylvian | Neck clipping | 0 | 0 | |||
| 3 | F | 60 | Rt. M2 | 0 | 0 | Saccular | Bifurcation | 1.6 | Y | 4 | Trans-sylvian | Neck clipping | 0 | 0 | ||
| 4 | F | 64 | Lt. M2 UR (SAH due to another AN) | 4 | 4 | Saccular | Bifurcation | 4.3 | Y | 3 | Trans-sylvian | Neck clipping | 4 | 4 | ||
| 5 | F | 62 | Lt. M2 UR | 0 | Saccular | Bifurcation | 5.2 | Trans-sylvian | Neck clipping | 0 | 0 | |||||
| 6 | F | 41 | Lt. M2 UR | 0 | Saccular | Bifurcation | 2.2 | Trans-sylvian | Neck clipping | 0 | 0 | |||||
| 7 | M | 48 | Rt. M2-M3 junction UR (Partial thrombosed) | 0 | Saccular | Bifurcation | 14* | Trans-sulcal | Y | Neck clipping additional bypass | Direct bypass with STA parietal branch | 0 | 0 | |||
| 8 | M | 59 | Rt. Distal M2 UR | 0 | Saccular | Bifurcation | 2.8 | Y | 3 | Trans-sylvian | Neck clipping | 0 | 0 | |||
| 9 | F | 31 | Rt. M2 R | 4 | 4 | Fusiform | 11† | Trans-sylvian | Failed clip‡ | Endovascular trapping | 4 | 6 | ||||
| 10 | F | 56 | Rt. MCA distal, fusiform (M3) | 0 | Fusiform | 11† | Trans-sylvian | Y | Proximal occlusion and bypass | Direct bypass with STA parietal branch | 0 | 0 | ||||
| 11 | F | 70 | Rt. M2 UR | 0 | Saccular | Bifurcation | 5.1 | Trans-sylvian | Neck clipping | 0 | 0 | |||||
| 12 | M | 51 | Rt. MCA M2 dissecting R | 2 | 1 | Dissecting | 15† | Trans-sylvian | Wrap clipping | Wrapping with encircling bemsheet and 3 clips | 0 | 0 | ||||
| 13 | F | 73 | Lt. M2 | 0 | 0 | Saccular | Sidewall | 5.6 | Trans-sylvian | Neck clipping | 0 | 0 | ||||
| 14 | F | 71 | Rt. M2 UA | 0 | 0 | Saccular | Bifurcation | 3 | Y | 3 | Trans-sylvian | Neck clipping | 0 | 0 | ||
| 15 | F | 62 | left M2 R | 4 | 4 | Fusiform | 4.1† | Trans-sylvian | Trapping | 2 clips | 4 | 6 | ||||
| 16 | M | 74 | Rt. M3 prox. UR | 0 | 0 | Saccular | Sidewall | 5.9 | Trans-sylvian | Y | Neck clipping | 0 | 0 |
REFERENCES
1. Acerbi F, Prada F, Vetrano IG, Falco J, Faragò G, Ferroli P, et al. Indocyanine green and contrast-enhanced ultrasound videoangiography: A synergistic approach for real-time verification of distal revascularization and aneurysm occlusion in a complex distal middle cerebral artery aneurysm. World Neurosurgery. 2019 May;125:277-84.


2. Baldoncini M, Wahjoepramono EJ, Wahjoepramono POP, Campero A, Justa A, Spetzler R, et al. Wrapping technique in fusiform aneurysms. Neurol Sci Neurosurg. 2020 2(1):111.

3. Baltacioğlu F, Cekirge S, Saatci I, Oztürk H, Arat A, Pamir N, et al. Distal middle cerebral artery aneurysms. Endovascular treatment results with literature review. Interv Neuroradiol. 2002 Dec;8(4):399-407.




4. Calvacante T, Derrey S, Curey S, Langlois O, Fréger P, Gérardin E, et al. Distal middle cerebral artery aneurysm: A proposition of microsurgical management. Neurochirurgie. 2013 Jun;59(3):121-7.


5. Dashti R, Hernesniemi J, Niemelä M, Rinne J, Lehecka M, Shen H, et al. Microneurosurgical management of distal middle cerebral artery aneurysms. Surg Neurol. 2007 Jun;67(6):553-63.


6. Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg. 1981 Feb;54(2):151-69.


7. Horiuchi T, Nakagawa F, Miyatake M, Iwashita T, Tanaka Y, Hongo K. Traumatic middle cerebral artery aneurysm: case report and review of the literature. Neurosurg Rev. 2007 Jul;30(3):263-7; discussion 267.



8. Horiuchi T, Tanaka Y, Takasawa H, Murata T, Yako T, Hongo K. Ruptured distal middle cerebral artery aneurysm. J Neurosurg. 2004 Mar;100(3):384-8.


9. Imada Y, Mihara C, Kawamoto H, Kurisu K. Dissection of the sylvian fissure in the trans-sylvian approach based on the morphological classification of the superficial middle cerebral vein. Neurol Med Chir (Tokyo). 2021 Dec;61(12):731-40.



10. Johnson HR, South JR. Traumatic dissecting aneurysm of the middle cerebral artery. Surg Neurol. 1980 Sep;14(3):224-6.

11. Joo SP, Kim TS, Choi JW, Lee JK, Kim YS, Moon KS, et al. Characteristics and management of ruptured distal middle cerebral artery aneurysms. Acta Neurochir (Wien). 2007 149(7):661-7.



12. Lee SH, Bang JS. Distal middle cerebral artery M4 aneurysm surgery using navigation-CT angiography. J Korean Neurosurg Soc. 2007 Dec;42(6):478-80.



13. Lee SJ, Shim YS, Park KY, Hong CK, Lee JW, Ahn JY. Clinical characteristics and surgical treatment of patients with distal middle cerebral artery aneurysms. Korean J Cerebrovasc Surg. 2008 10(3):508-12.
14. Maekawa H, Hadeishi H. Venous-preserving Sylvian dissection. World Neurosurg. 2015 Dec;84(6):2043-52.


15. Park SH, Yim MB, Lee CY, Kim E, Son EI. Intracranial fusiform aneurysms: It’s pathogenesis, clinical characteristics and managements. J Korean Neurosurg Soc. 2008 Sep;44(3):116-23.



16. Piepgras DG, McGrail KM, Tazelaar HD. Intracranial dissection of the distal middle cerebral artery as an uncommon cause of distal cerebral artery aneurysm. J Neurosurg. 1994 May;80(5):909-13.


17. Rinne J, Hernesniemi J, Niskanen M, Vapalahti M. Analysis of 561 patients with 690 middle cerebral artery aneurysms: Anatomic and clinical features as correlated to management outcome. Neurosurgery. 1996 Jan;38(1):2-11.


18. Rodríguez-Hernández A, Lawton MT. Flash fluorescence with indocyanine green videoangiography to identify the recipient artery for bypass with distal middle cerebral artery aneurysms: Operative technique. Neurosurgery. 2012 Jun;70(2 Suppl Operative):209-20.

19. Seo D, Lee SU, Oh CW, Kwon OK, Ban SP, Kim T, et al. Characteristics and clinical course of fusiform middle cerebral artery aneurysms according to location, size, and configuration. J Korean Neurosurg Soc. 2019 Nov;62(6):649-60.




20. Sotero FD, Rosário M, Fonseca AC, Ferro JM. Neurological complications of infective endocarditis. Curr Neurol Neurosci Rep. 2019 Mar;19(5):23.



21. Sturiale CL, Brinjikji W, Murad MH, Cloft HJ, Kallmes DF, Lanzino G. Endovascular treatment of distal anterior cerebral artery aneurysms: Single-center experience and a systematic review. AJNR Am J Neuroradiol. 2013 Dec;34(12):2317-20.



22. Sung SK, Cho WH, Lee SW, Choi CH. Surgical treatment of distal middle cerebral artery aneurysms. Korean J Cerebrovasc Surg. 2004 6(1):45-9.
23. Tayebi Meybodi A, Huang W, Benet A, Kola O, Lawton MT. Bypass surgery for complex middle cerebral artery aneurysms: An algorithmic approach to revascularization. J Neurosurg. 2017 Sep;127(3):463-79.


24. Tsutsumi K, Horiuchi T, Nagm A, Toba Y, Hongo K. Clinical characteristics of ruptured distal middle cerebral artery aneurysms: Review of the literature. J Clin Neurosci. 2017 Jun;40:14-7.


25. Varma S, Banh L, Smith P. Traumatic aneurysm of the cortical middle cerebral artery. BMJ Case Rep. 2017 Feb;2017:bcr 2017219301.



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,157 View
- 37 Download
- ORCID iDs
-
Sung-Tae Kim

https://orcid.org/0000-0002-3737-3850 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



