 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 26(1); 2024 > Article |
|
Abstract
Dural arteriovenous fistula (DAVF) is a rare condition affecting approximately 1.5% of 1,000,000 individuals annually. It frequently occurs in the transsigmoid and cavernous sinuses. An isolated sigmoid sinus is extremely rare and is treated by performing transfemoral transvenous embolization along the opposite transverse sinus.
A 69-year-old woman presented with asymptomatic Borden type III/Cognard type III DAVF involving an isolated sigmoid sinus. She underwent a staged operation in which a navigation system was used to expose the sigmoid sinus in the operating room before transferring the patient to the angio suite for transvenous embolization.
Various modalities have been used to treat DAVF, including surgical disconnection, transarterial embolization, transvenous embolization, and stereotactic radiosurgery. However, treating DAVF cases where the affected sinus is isolated can be challenging because an easily accessible surgical route may not be available. In this case, direct sinus cannulation and transvenous embolization were the most effective treatments.
Dural arteriovenous fistula (DAVF) is a rare type of cerebrovascular malformation, accounting for only 10-15% of cases [9]. Intracerebral hemorrhage is a severe complication of DAVF associated with poor outcome. Among the types of DAVF, the isolated type is high grade owing to potential drainage into the cortical venous system [1]. Several studies indicate that this type of DAVF frequently causes hemorrhagic complications [3,4,6]. Despite advances in endovascular technology and stereotactic radiosurgery, the treatment of isolated-type DAVF remains challenging for neurosurgeons owing to increased risk of bleeding from multiple feeding arteries during open surgery, limited accessibility to endovascular treatment, and potentially incomplete treatment via stereotactic radiosurgery. Here, we report a case of a staged operation to treat DAVF of an isolated sigmoid sinus, which involved exposure of the sinus via minimally invasive craniectomy in the operating room, followed by embolization using a transvenous approach in the angio suite.
A 69-year-old female patient was referred from the Neurology Department with abnormal findings on magnetic resonance angiography (MRA) images. Upon neurological examination, no symptoms of tinnitus, vomiting, or altered mental state were noted, and her consciousness was alert with only mildly impaired cognitive function. On radiological examination, T2-weighted imaging revealed enlarged pial vessels in the subarachnoid space (Fig. 1A), and MRA revealed arteriovenous shunting into the isolated sigmoid sinus and cortical veins (Fig. 1B). Catheter digital subtraction angiography (DSA) revealed a right-sided DAVF involving the sigmoid sinus, with multiple instances of cortical vein reflux fed by the transosseous branches and posterior meningeal branches of the occipital artery and the parietal branch of the middle meningeal artery (Fig. 2A, 2B). DSA was performed to assess the extent of retrograde cortical vein reflux and venous drainage (Fig. 2C, 2D). The ipsilateral transverse sinus and jugular vein were not visualized, indicating a pure isolated sigmoid sinus DAVF with multiple instances of cortical vein reflux, classified as Borden type III or Cognard type III. No abnormal shunting was observed in any of the other arteries. Because the lesion was inaccessible via a conventional transfemoral transvenous approach, transvenous embolization via direct cannulation of the sigmoid sinus was planned for complete obliteration of the fistula. In the operating room, under general anaesthesia, a small craniectomy was performed using preoperative CT angiography images and the Stryker neuronavigation system (Stryker Instruments, Kalamazoo, MI, USA) (Fig. 3A). The sigmoid sinus was exposed within the small craniectomy, and bleeding was controlled using bone wax and fibrinogen/thrombin-based collagen fleece (TachoCombⓇ, CSL Behring, Tokyo, Japan) (Fig. 3B). The patient was then transferred to the angio suite, and a 5-French sheath was placed in the left femoral artery. Using visual surveillance and roadmap guidance, the right sigmoid sinus was punctured using a micropuncture needle, and a micropuncture sheath was sequentially placed under fluoroscopic guidance. A microcatheter (Headway-17TM, MicroVention, Tustin, CA, USA) was positioned appropriately for embolization at the fistula point (Fig. 4). Subsequently, the sinus was embolized using multiple detachable packing coils. The microcatheter was carefully retracted while densely packing the sigmoid sinus with coils from the superior to inferior regions. Although complete embolization with coils alone was initially anticipated, a post-embolization angiogram following the placement of 10 detachable packing coils of various sizes (MicroVention, Tustin, CA, USA) revealed a reduction in the flow limited to the sinus and fistula areas. To achieve complete obliteration of the fistula, glue embolization was performed with OnyxⓇ (ev3, Irvine, CA, USA) (Fig. 5). The patient was discharged without complications.
DAVF is a type of vascular malformation characterized by abnormal connections between the intracranial arteries and the dural leaflets of the venous sinuses. It accounts for approximately 10%-15% of all intracranial vascular malformations [9]. Its etiology is mostly unknown, although dural sinus thrombosis, trauma, infection, or a prior craniotomy have been reported as potential causes [12]. DAVF can occur in various locations, including the superior sagittal sinus, tentorial cerebelli, petrosal process, and spinal dura. Supratentorial locations are more commonly reported than infratentorial locations, with the transverse sigmoid sinus being the most common [7]. The manifestation in the present case was extremely rare in that it involved a single isolated sigmoid sinus, which posed several limitations for treatment.
Pure sigmoid sinus DAVF can be anatomically more challenging to access than transverse sigmoid sinus DAVF. They are often located deep within the sinuses, and in areas that are difficult to access. This decreases the accessibility of treatment and increases the risk of tissue damage. In the case of a purely isolated sigmoid sinus DAVF, transvenous embolization via the transverse sinus by approaching the contralateral sigmoid sinus is not possible. Additionally, the fistula point in an isolated sigmoid sinus DAVF is smaller than that in a transverse sigmoid sinus DAVF. In such cases, surgical exposure of the sinuses is difficult. Treating isolated sigmoid sinus DVAFs by performing stereotactic radiosurgery is also challenging because of the relatively small radiation exposure area. A PubMed search in English using the keyword “isolated sigmoid sinus” did not yield any directly correlated case reports or clinical articles. Similarly, Google Scholar yielded no significant results. Our case highlights the importance of addressing the risk of hemorrhage due to drainage through the cortical veins in patients with isolated DAVF [1]. Our principal goal was to prevent hemorrhage by complete obliteration of the fistula.
In our case, stereotactic radiosurgery was deemed unsuitable because of the low cure rates and the latency period required to achieve obliteration. Microsurgical treatments such as the interruption of leptomeningeal venous drainage, skeletonization, direct sinus packing, and sinus reconstruction have high cure rates with acceptable morbidity and mortality [8,10,15]. However, these treatments carry a risk of excessive bleeding owing to multiple feeding arteries, which was a major concern in the present case.
In recent years, endovascular therapy has emerged as a first-line treatment option for most cases of DAVF, particularly in patients with multiple comorbidities who are at a high risk of complications associated with open surgery. Transarterial embolization using liquid embolic materials has also become a feasible modality for treating DAVF [5], although it has a post-procedural occlusion rate of 30% [2]. In the present case, the key to treating the DAVF centered on the occlusion of the fistula point was that transarterial embolization via small branches of the occipital artery was not feasible for complete obliteration, given the concerns of infarction owing to unwanted embolization. Transarterial embolization of the parietal branch of the middle meningeal artery may also be a good treatment option. However, this was not attempted in the present case because it was not the main feeder artery [13].
Transvenous embolization, which allows direct access to the fistula point, is often preferred in cases of DAVF involving an isolated sinus. However, lack of accessibility can present challenges for surgeons. Various methods have been introduced, including direct access through an occluded sinus [11]. However, this is associated with potential complications, such as perforation of the sinus. Komiyama et al. introduced access to a DAVF involving an isolated transverse sigmoid sinus on the contralateral side [11]. In our case, this method was unsuitable because of the lack of a transverse sinus.
Several reports have described an approach involving a small craniectomy for sinus exposure combined with transvenous embolization via direct sinus puncture [14]. Although drilling over the sinus carries the risk of perforation, neuronavigation technology can reduce this risk [2]. We were constrained by the lack of a hybrid operating system in our institution. Alternatively, we initially performed a craniotomy using a neuronavigation system in the operating room to ensure the accuracy of the burr hole and to gather information regarding the DAVF and surrounding bony structures. Subsequently, the patient was transferred to the angio suite for transvenous embolization. It was unnecessary to transfer the patient to a facility with a hybrid operating system to perform both the surgical and endovascular procedures. Combining surgical and endovascular methods is a reliable way to manage challenging cases of DAVF with an isolated sinus. Given the development of sophisticated neuronavigation and hybrid operating systems, the treatment outcomes for DAVF are promising.
A DAVF involving an isolated sinus remains a challenge for healthcare practitioners. However, combined surgical and endovascular treatments can completely obliterate malformations. Advances in technology, such as neuronavigation and hybrid operating systems, have helped reduce the complications associated with these procedures. Therefore, a combined treatment approach is recommended as the first-line therapy for DAVF involving an isolated sinus with limited accessibility. An individualized treatment plan must be developed based on the specific characteristics and location of the DAVF as well as the overall health of the patient. A multidisciplinary approach involving a team of neurosurgeons, neurointerventionists, and other specialists can enhance the chances of successful outcomes.
Fig. 1.
Preoperative MRI and MRA. (A) Brain MRI T2 image showing multiple areas with low signal intensity in the subarachnoid space without other abnormal findings in the brain parenchyma. (B) MRA demonstrating an irregular and tortuous vascular structure around the right sigmoid sinus. MRI, magnetic resonance imaging; MRA, magnetic resonance angiography
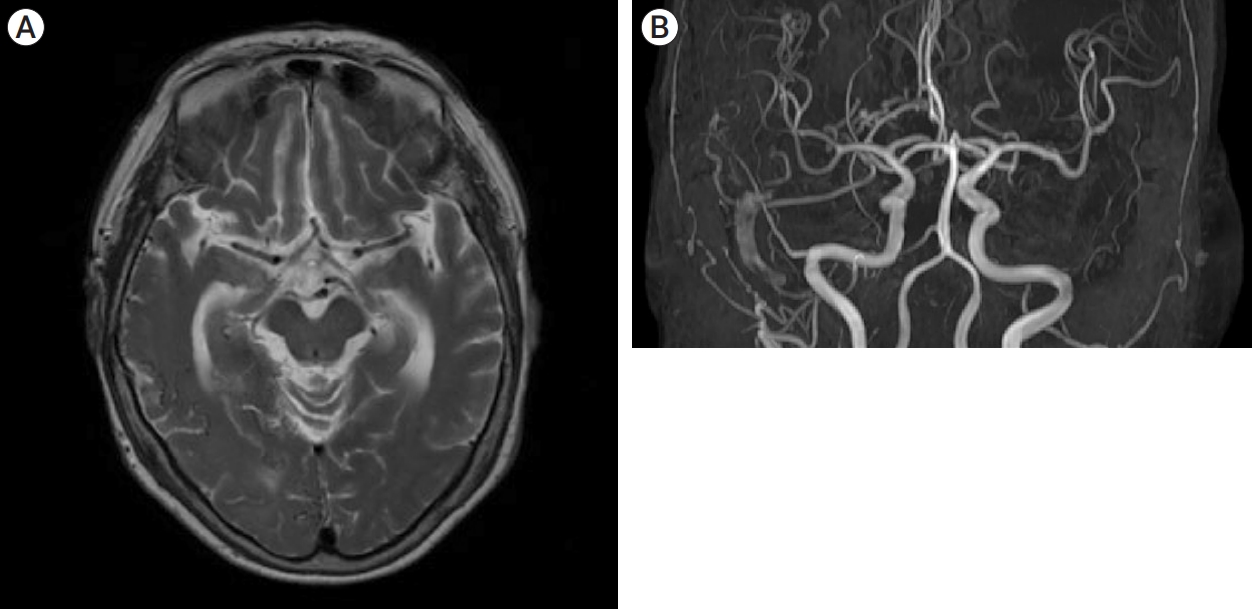
Fig. 2.
Preoperative transfemoral angiography. (A and B) External carotid angiogram showing the DAVF. The sigmoid sinus appears in the early arterial phase with multiple feeding occipital artery branches, the parietal branch of the middle meningeal artery, and cortical vein refluxes. (C and D) Delayed venous phase angiogram demonstrating extensive cortical vein refluxes without opacification of the ipsilateral transverse sinus or jugular vein, indicating an isolated sigmoid sinus. DAVF, dural arteriovenous fistula
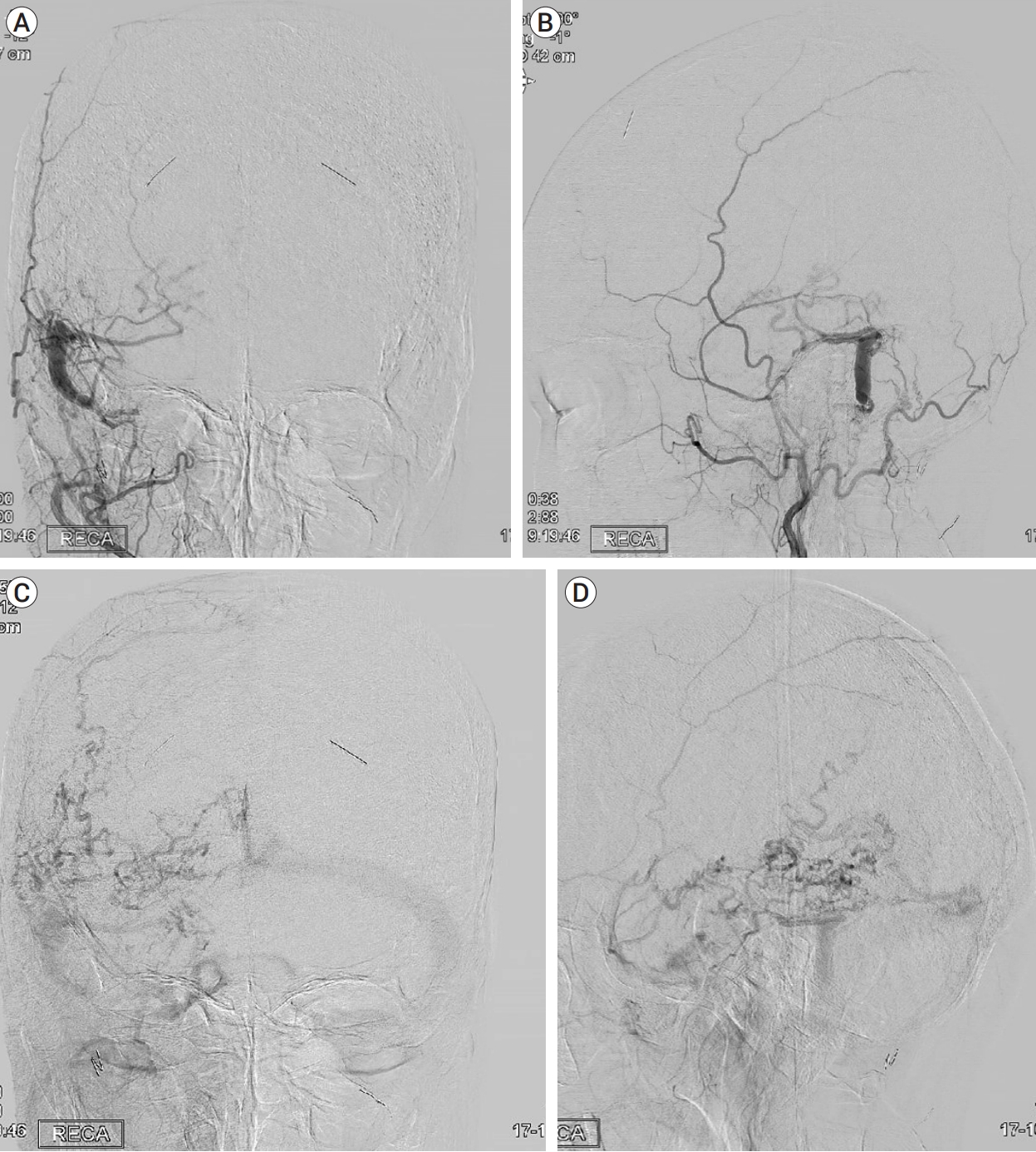
Fig. 3.
Intraoperative photograph demonstrating. (A) Planning the craniectomy using a neuronavigation system. (B) Exposure of the sigmoid sinus (black arrowhead) after creating a small craniectomy.
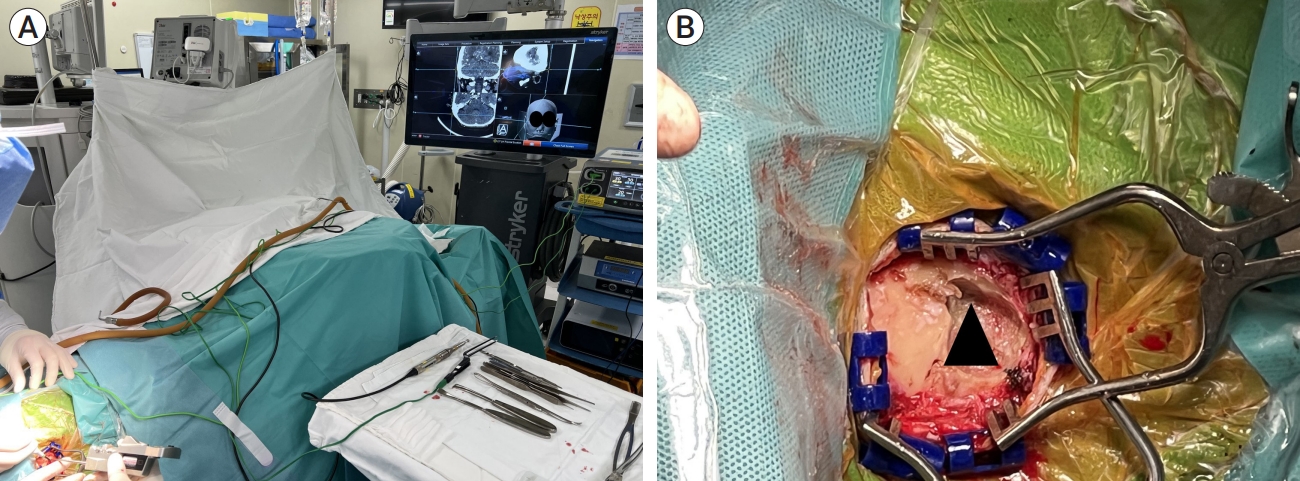
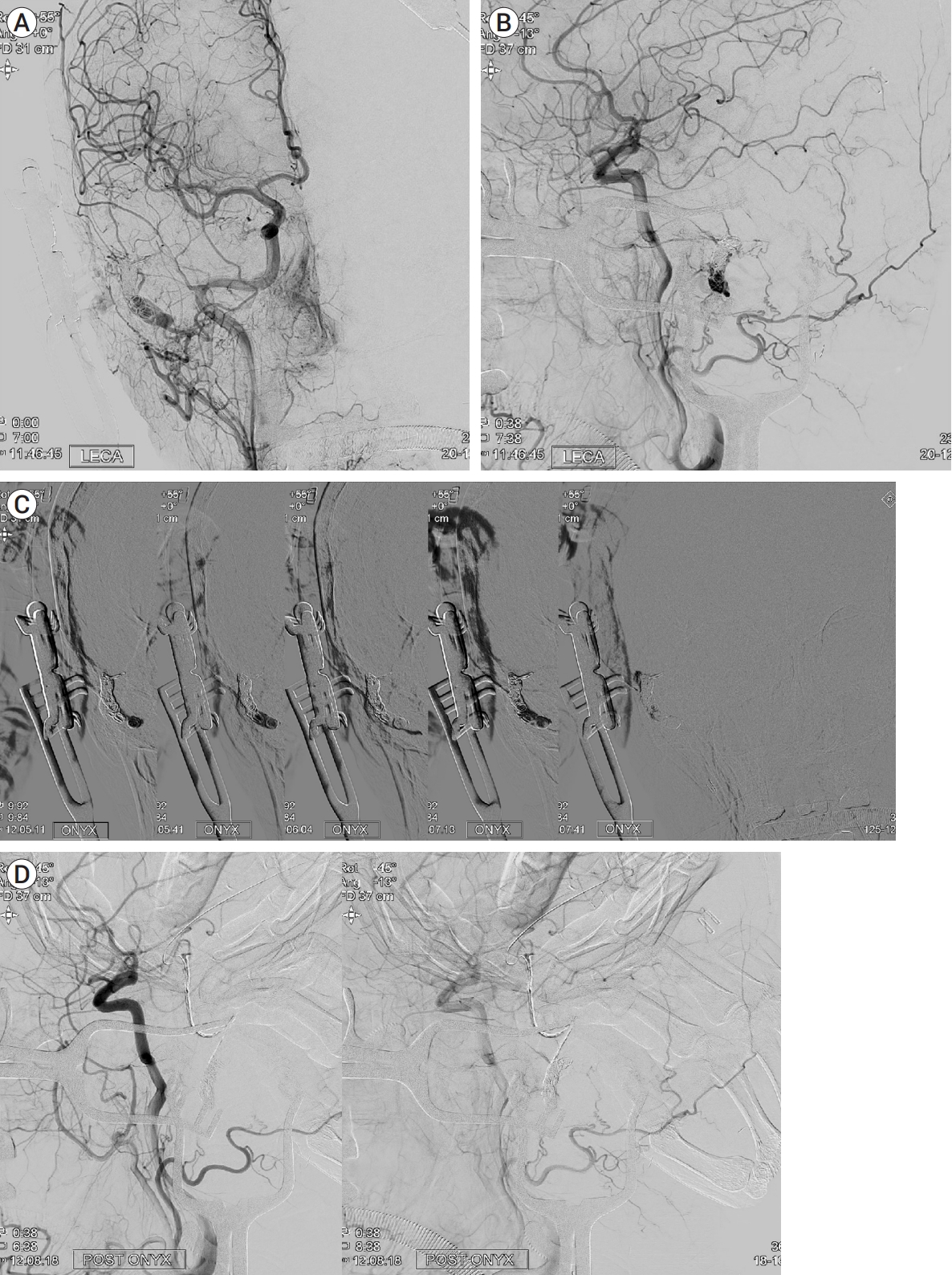
Fig. 4.
Intraoperative photograph and right common carotid angiogram. (A) Photograph demonstrating the position of the microcatheter and micropuncture sheath. (B and C) Navigation of the microcatheter over a microwire into the right isolated sigmoid sinus under fluoroscopic guidance.

Fig. 5.
(A and B) Angiogram showing partial occlusion of the isolated sigmoid sinus with the feeding artery after adding nine packing coils. (C) Sequential Onyx cast filling the sigmoid sinus and feeding artery, with a remnant fistula point. (D) Final early and late phase angiogram demonstrating complete obliteration of the DAVF. DAVF, dural arteriovenous fistula
REFERENCES
1. Baharvahdat H, Ooi YC, Kim WJ, Mowla A, Coon AL, Colby GP. Updates in the management of cranial dural arteriovenous fistula. Stroke Vasc Neurol. 2019 Nov;5(1):50-8.



2. Cheng AC, Li EY, Chan TC, Wong AC, Chan PC, Poon WW, et al. Hybrid procedure for orbital venous malformation in the endovascular operation room. Eye (Lond). 2015 Aug;29(8):1069-75.




3. Choi JH, Jo KI, Kim KH, Jeon P, Yeon JY, Kim JS, et al. Early rebleeding of intracranial dural arteriovenous fistulas after an intracranial hemorrhage. Acta Neurochir (Wien). 2017 Aug;159(8):1479-87.



4. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995 Mar;194(3):671-80.


5. Cognard C, Januel AC, Silva NA Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: New management using Onyx. AJNR Am J Neuroradiol. 2008 Feb;29(2):235-41.



6. Duffau H, Lopes M, Janosevic V, Sichez JP, Faillot T, Capelle L, et al. Early rebleeding from intracranial dural arteriovenous fistulas: Report of 20 cases and review of the literature. J Neurosurg. 1999 Jan;90(1):78-84.


7. Elhammady MS, Ambekar S, Heros RC. Epidemiology, clinical presentation, diagnostic evaluation, and prognosis of cerebral dural arteriovenous fistulas. Handb Clin Neurol. 2017 143:99-105.


8. Endo S, Kuwayama N, Takaku A, Nishijima M. Direct packing of the isolated sinus in patients with dural arteriovenous fistulas of the transverse-sigmoid sinus. J Neurosurg. 1998 Mar;88(3):449-56.


9. Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: Classification, imaging findings, and treatment. AJNR Am J Neuroradiol. 2012 Jun;33(6):1007-13.



10. Gross BA, Du R. Surgical treatment of high grade dural arteriovenous fistulae. J Clin Neurosci. 2013 Nov;20(11):1527-32.


11. Komiyama M, Ishiguro T, Matsusaka Y, Yasui T, Nishio A. Nishio A. Transfemoral, transvenous embolisation of dural arteriovenous fistula involving the isolated transverse-sigmoid sinus from the contralateral side. Acta Neurochir (Wien). 2002 Oct;144(10):1041-6; discussion 1046.



12. Micieli JA, Derkatch S, Pereira VM, Margolin EA. Development of dural arteriovenous fistulas after cerebral venous sinus thrombosis. J Neuroophthalmol. 2016 Mar;36(1):53-7.


13. Murayama Y, Arakawa H, Ishibashi T, Kawamura D, Ebara M, Irie K, et al. Combined surgical and endovascular treatment of complex cerebrovascular diseases in the hybrid operating room. J Neurointerv Surg. 2013 Sep;5(5):489-93.


-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,422 View
- 23 Download
- ORCID iDs
-
Jong-Hyun Park

https://orcid.org/0009-0000-4789-4521 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



