 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 25(4); 2023 > Article |
|
Abstract
Bilateral posterior communicating (pComm) artery aneurysms represent only 2% of mirror intracranial aneurysms. Usually, these are surgically approached through bilateral craniotomies for clipping. We present the case of a 50-year-old female presenting with headache and horizontal diplopia. Neurological examination revealed a left oculomotor palsy, with no other neurological deficits. Imaging studies revealed bilateral aneurysmatic lesions in both internal carotid arteries (ICA). A conventional left pterional approach was planned in order to treat the symptomatic aneurysm, and, if deemed feasible, a contralateral clipping through the same approach. The procedure was performed in a hybrid operating room (HOR), performing an intraoperative digital subtraction angiography (DSA) and roadmapping assistance during dissection and clipping. Transoperatively, a post-fixed optic chiasm was identified, with a wide interoptic space, which allowed us to perform the contralateral clipping through a unilateral approach. This technique for clipping bilateral pComm aneurysms can be performed when the proper anatomical features are met.
Multiple intracranial aneurysms, corresponding to 15-25% of cerebral aneurysms, are relatively frequent among the vascular diseases of the central nervous system [3]. Posterior communicating (pComm) aneurysms represent 15 to 25% of intracranial aneurysms [10]. Bilateral pComm aneurysms (“mirror aneurysms”) are rare, representing only 2% of the mirror intracranial aneurysms, thus being a true neurosurgical challenge [1], with only a few cases reported in the current literature [7]. In this article, we present a patient with mirror pComm aneurysms in which both lesions were treated through a single approach, followed by a brief review of the literature.
A 50-year-old female patient with no previous medical background was admitted to our institution after presenting recurrent episodes of non-specific headache and horizontal diplopia. Neurological examination revealed a Glasgow Coma Scale (GCS) of 15 (M6, V5, O4), and a left oculomotor palsy, with no further disturbances. Non-contrast computed tomography (CT) and an angioCT scans revealed bilateral aneurysmatic lesions in both internal carotid arteries (ICA) communicating segments. A digital subtraction angiography (DSA) was performed in order to get a better anatomical definition of both aneurysms (Fig. 1). We decided to perform a left pterional approach in order to gain access to the symptomatic lesion at first instance, and if anatomical findings were optimal, a contralateral clipping would be sought for the right aneurysm. It is essential to mention that this procedure was performed in a hybrid operating room (HOR) with DSA before clipping, roadmapping assistance during both dissection and clipping, and an immediate postclipping DSA to assess distal vascular permeability and vasospasm.
During subarachnoid dissection, a post-fixed optic chiasm with a wide interoptic space was identified (Fig. 2), which allowed a complete dissection of the arachnoid planes, with complete visualization of the contralateral aneurysm’s neck and collateral arteries of the contralateral ICA (pComm and anterior choroidal artery) (Fig. 3). After thorough, the ipsilateral aneurysm was clipped with no difficulty, assessing patency of the ICA branches (Fig. 4) with DSA (Fig. 5). Both aneurysms were permanently clipped with a 7 mm straight clip. The patient’s postoperative course was uneventful, with a sequel left oculomotor palsy.
Multiple intracranial aneurysms represent around 15-30% of all aneurysms [9]. Mirror aneurysms represent about 2 to 12% of the latter, being the pComm location the third most frequent [6]. Previous studies have described the site of the lesion and the clinical characteristics of mirror aneurysms, however, results differ. Meissner et al. [6] found that mirror aneurysms are more extensive than single aneurysms. In contrast, Lee et al. [4] found that mirror aneurysms are smaller than their counterparts.
Risk factors associated with mirror aneurysms are female sex, smoking, alcohol consumption, and genetic variables that directly influence their growth because of the hemodynamic stress in the aneurysm wall [2,5,10].
Although studies have fully analyzed the clinical characteristics, risk factors, and incidence of mirror aneurysms, there is not a consensus about the appropriate approach to these lesions. Many authors have proposed various approaches for bilateral pComm aneurysms. Some include endovascular therapy for both lesions, endovascular therapy for the non-ruptured lesion and clipping for the ruptured one, or clipping by bilateral approaches [8]. These approaches are selected whereas there is a ruptured aneurysm, its location, the size of its neck, and the patient’s neurological condition. However, the criteria for treatment need to be better defined as there is still controversy about the appropriate management.
Unilateral approaches for bilateral pComm aneurysms have been described only in case reports [7]. However, most neurosurgeons prefer unilateral approaches for unilateral lesions without rupture because of the manipulation and mobilization of the surrounding structures. Likewise, the single approach is technically complex because the angle of view of the contralateral neck can be slight. In addition, cerebral edema can make managing the surgical space more challenging in ruptured aneurysms.
In our case, we can observe how the unilateral approach can be implemented in selected cases of bilateral pComm aneurysms because the wide interoptic space allows us to visualize the neck of the contralateral aneurysm achieving a correct clipping. Some anatomical factors that allow complete visualization of the contralateral neck are a wide interoptic space and a post-fixed chiasm. However, it should be mentioned that only during surgery can we judge whether these anatomical factors and cerebral edema can provide enough space to maneuver on the contralateral side and perform the clipping. Future studies should be performed using preoperative magnetic resonance image measurements to determine whether we can use the unilateral approach routinely.
We consider this technique is less expensive than bilateral endovascular approaches and less morbid than bilateral craniotomies because the surgical time is reduced and a single incision is made. Likewise, it is unnecessary to expose the patient to two surgical times for combined approaches (endovascular and clipping at different times).
Unilateral approaches for bilateral pComm aneurysms can be feasible, safe, and less expensive than other approaches. However, it is imperative to remember that visualization of the contralateral neck of the aneurysm, grade of cerebral edema, and experience of the neurosurgeon are factors that carry out a good clipping. In addition, it is necessary to have full vascular anatomical knowledge and the use of the technological tools available to perform effective and safe surgery.
Fig. 1.
Preoperative DSA showing bilateral pComm aneurysms. (A) Right pComm aneurysm. (B) Left pComm aneurysm. White arrows representing the location of both aneurysms. DSA, digital subtraction angiography; pComm, posterior communicating
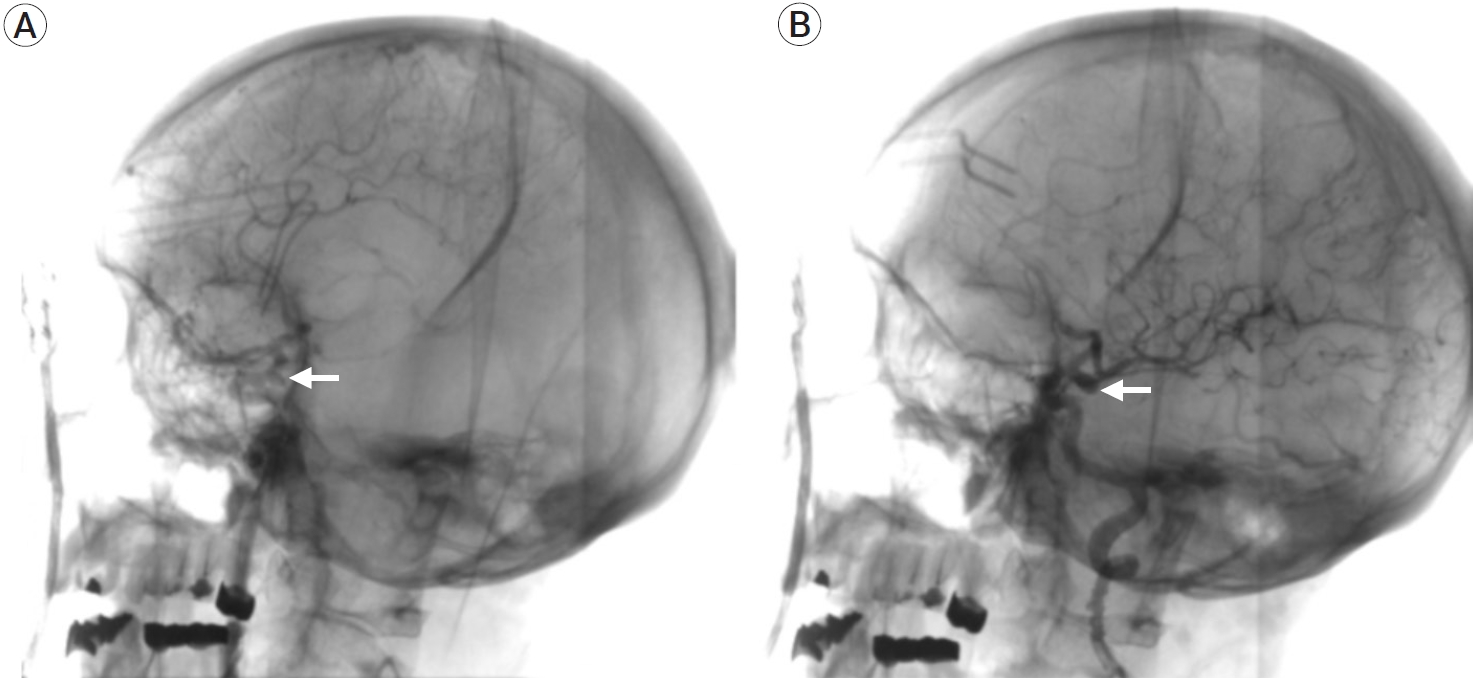
Fig. 2.
Artist drawing illustrating the post-fixed optic chiasm and a wide interoptic space, allowing a complete view of the neck of the contralateral pComm aneurysm. pComm, posterior communicating
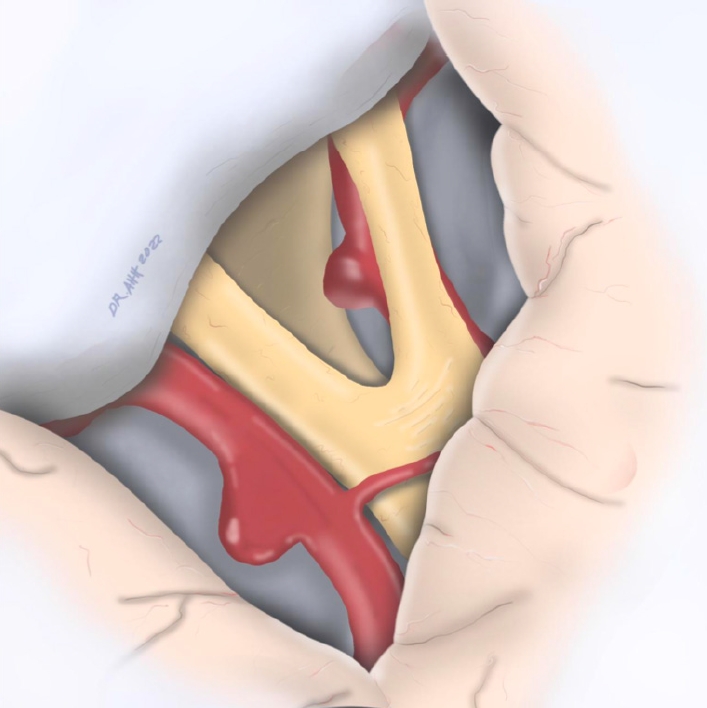
Fig. 3.
Contralateral pComm aneurysm clipping. (A) Operative view. 1. Left ICA. 2. Contralateral aneurysm clip. 3. Right ICA and right aneurysm neck. 4. Left ICA bifurcation. 5. Right optic nerve. 6. Left optic nerve. (B) Artist drawing illustration of the contralateral pComm aneurysm clipping. pComm, posterior communicating; ICA, internal carotid arteries

Fig. 4.
Ipsilateral pComm aneurysm clipping. (A) Operative view. 1. Ipsilateral pComm aneurysm’s dome. 2. Ipsilateral clip. 3. Contralateral clip. 4. Left ICA. (B) Artist drawing illustration of the ipsilateral pComm aneurysm clipping and the contralateral pComm aneurysm clipped before. pComm, posterior communicating; ICA, internal carotid arteries

REFERENCES
1. Choi HH, Cho YD, Yoo DH, Lee J, Mun JH, An SJ, et al. Intracranial mirror aneurysms: Anatomic characteristics and treatment options. Korean J Radiol. 2018 Sep-Oct;19(5):849-58.




2. Ellamushi HE, Grieve JP, Jäger HR, Kitchen ND. Risk factors for the formation of multiple intracranial aneurysms. J Neurosurg. 2001 May;94(5):728-32.


3. Kaminogo M, Yonekura M, Shibata S. Incidence and outcome of multiple intracranial aneurysms in a defined population. Stroke. 2003 Jan;34(1):16-21.


4. Lee YJ, Parreira T, Matouk CC, Menezes R, Mandell DM, terBrugge KG, et al. Clinical characteristics and preferential location of intracranial mirror aneurysms: A comparison with non-mirror multiple and single aneurysms. Neuroradiology. 2015 Jan;57(1):35-40.



5. Lu HT, Tan HQ, Gu BX, Wang W, Li MH. Risk factors for multiple intracranial aneurysms rupture: A retrospective study. Clin Neurol Neurosurg. 2013 Jun;115(6):690-4.


6. Meissner I, Torner J, Huston J, Rajput ML, Wiebers DO, Jones LK Jr, et al. Mirror aneurysms: A reflection on natural history. J Neurosurg. 2012 Jun;116(6):1238-41.



7. Wang J, Xu F. Unilateral supraorbital approach to clip bilateral posterior communicating artery aneurysms: 2-dimensional operative video. World Neurosurg. 2018 Nov;119:256.


8. Wang WX, Xue Z, Li L, Wu C, Zhang YY, Lou X, et al. Treatment strategies for intracranial mirror aneurysms. World Neurosurg. 2017 Apr;100:450-8.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,240 View
- 24 Download
- ORCID iDs
-
Ricardo Marian-Magaña

https://orcid.org/0000-0002-0518-9629 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



