Retreatment of a recurrent giant aneurysm of the internal carotid artery after treatment with a flow-diverting stent
Article information
Abstract
Flow-diverting stents (FDSs) have proven advantageous for the treatment of large, fusiform, and dissecting aneurysms that are otherwise difficult to treat. Retreatment strategies for recurrent large or giant aneurysms after FDSs are limited to overlapping implantation of an additional FDS or definitive occlusion of the parent vessel. We report a recurrent giant aneurysm that was initially treated with an FDS with coils and was successfully treated with an additional FDS. Visual symptoms due to the mass effect of the recurrent aneurysm were completely resolved, and follow-up digital subtraction angiography revealed complete obliteration of the aneurysm. Additional FDS implantation for the retreatment of incompletely occluded aneurysms after the initial FDS treatment may be feasible and safe. Further studies are required to validate these results.
INTRODUCTION
Currently, many endovascular treatments are being performed to treat cerebral aneurysms. However, there are still issues with the durability of treatment and the likelihood of recurrence [13]. Even after general stent-assisted coil insertion is performed, the recurrence rate is as high as 14.9% [12].
A flow-diverting stent (FDS) is an endovascular treatment that is useful for the treatment of complex uncommon aneurysms such as giant, blister, and dissecting aneurysms, which are also prone to recurrence [5,11,16]. In addition, clinical evidence shows that an FDS has a higher complete occlusion rate than stent-assisted coils [8]. An FDS can provide more durable aneurysm occlusion when compared with other techniques such as conventional, balloon-assisted, or stent-assisted coiling, and still offers acceptable morbidity and mortality rates in these complex aneurysms. However, an FDS can lead to bleeding and ischemic complications, which are significant causes of neurological morbidity and mortality [2,9].
Retreatment of previously stented aneurysms is challenging owing to its efficacy and safety [10]. The risk of rupture or re-rupture of recurrent aneurysms after an FDS is uncertain. Additionally, the retreatment of recurrent aneurysms after an FDS is rare and has technical limitations. The dense mesh design and high metal coverage of the FDS make microcatheter re-selection into the aneurysm sac impossible. Therefore, retreatment strategies for recurrent aneurysms after an FDS are limited to overlapping implantation of more FDSs or definitive occlusion of the parent vessel. Here, we report a recurrent giant aneurysm that was initially treated with an FDS with coils before successfully being treated with an additional FDS.
CASE DESCRIPTION
An incidental giant aneurysm of the right internal carotid artery (ICA) with a maximum diameter of approximately 26.3 mm was found in a 55-year-old man treated for right middle cerebral artery (MCA) infarction at another hospital (Fig. 1). Due to the right MCA infarction, the patient had minimal left hemiparesis and left homonymous hemianopsia, but was independent, with a modified Rankin Scale (mRS) score of 2. Preprocedural dual antiplatelet agents (aspirin 100 mg Qd and clopidogrel 75 mg Qd) had been administered due to cerebral infarction. After 3 weeks, the giant ICA aneurysm was treated by a FDS (Surpass Evolve; 5.0 mm×20 cm; Stryker Neurovascular, Kalamazoo, MI, USA), along with additional partial coil insertion at the other hospital.
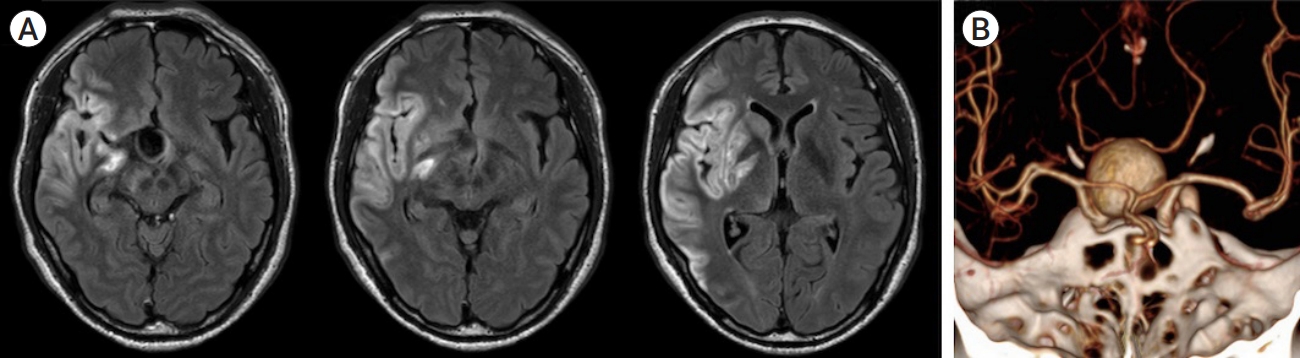
Radiological findings from another hospital. (A) Right middle cerebral artery infarction was seen on magnetic resonance images. (B) Computed tomography angiography revealed an incidental giant aneurysm on the right internal carotid artery with a maximum diameter of approximately 26.3 mm.
After 3 months, however, the patient’s visual field gradually began to narrow, and he came to our hospital with near-blinding. Visual field examination revealed that the bitemporal hemianopsia overlapped with pre-existing left homonymous hemianopsia (Fig. 2A). In the visual acuity test, only hand motion was detected in the right eye and 30/100 was detected in the left eye. On follow-up MRI, the aneurysm size increased, with a mass effect present on the optic nerves (Fig. 2B). As the size of the aneurysm increased, the third ventricle was blocked and the lateral ventricles slightly increased in size. As the aneurysm grew, the optic chiasm became compressed by the mass effect, causing bitemporal hemianopsia. Digital subtraction angiography (DSA) was performed and recurrence was observed in the neck of the aneurysm (Fig. 2C). The diameters of the proximal and distal ICA were 4.68 mm and 3.24 mm, respectively.

Three weeks after the cerebral infarction, the giant aneurysm was treated by a flow diverting stent (Surpass Evolve, 5.0 mm×20 cm;Stryker Neurovascular, Kalamazoo, MI, USA) and additional partial coil insertion at the other hospital. After 3 months, the patient’s visual field gradually began to narrow, and he came to our hospital near blindness. (A) Visual field examination revealed that bitemporal hemianopsia overlapped pre-existing left homonymous hemianopsia. (B) On the follow-up magnetic resonance images, the size of the aneurysm increased with a mass effect on the optic nerves. As the aneurysm grew, the optic chiasm was compressed by the mass effect, causing the bitemporal hemianopsia. (C) Digital subtraction angiography was performed, and a recurrence was observed in the neck of the aneurysm.
Retreatment was performed with an FDS (Surpass Evolve; 4.5 mm×20 cm; Stryker Neurovascular, Kalamazoo, MI, USA) deployed inside the previous FDS. Six months after the retreatment, the bitemporal hemianopsia improved and the visual field widened (Fig. 3A). In addition, the visual acuity of the right eye improved from only hand motion to 15/100. Follow-up DSA confirmed the complete obliteration of the aneurysm (Fig. 3B). Dual antiplatelet agents were maintained for 12 months after the procedure and were changed to aspirin monotherapy for life-long due to cerebral infarction.
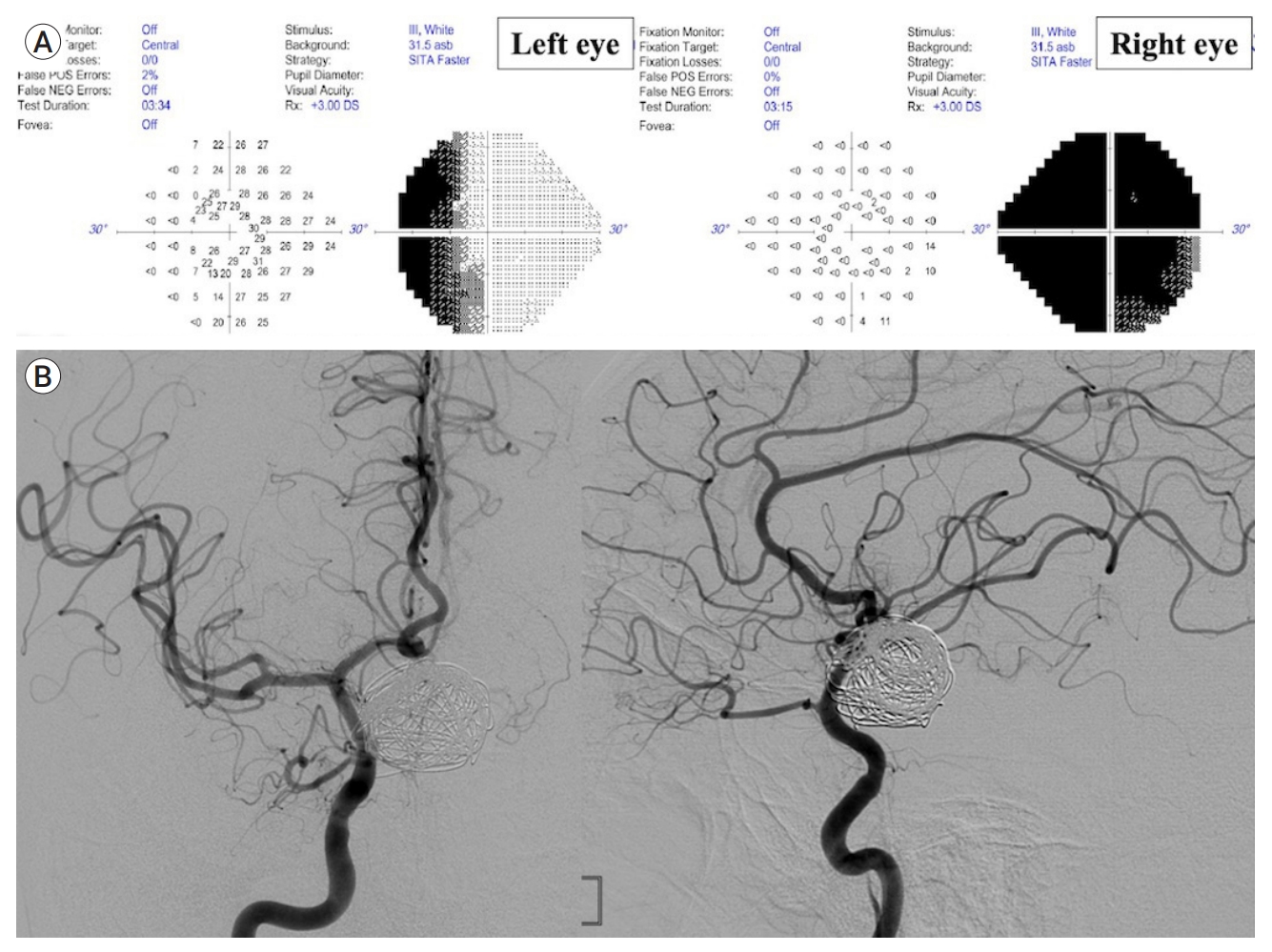
Six months after retreatment with a flow diverting stent (Surpass Evolve, 4.5 mm×20 cm, Stryker Neurovascular, Kalamazoo, MI, USA) deployed inside the previous flow diverting stent, (A) the bitemporal hemianopsia had improved, the visual field became wider, and (B) complete obliteration was achieved on the follow-up digital subtraction angiography.
DISCUSSION
Here, we report the case of a recurrent giant aneurysm after FDS treatment with partial coils. The size of the aneurysm increased with the mass effect on the optic nerves and the third ventricle, causing bitemporal hemianopsia and an increase in lateral ventricle size. Although the risk of rupture of recurrent aneurysms after an FDS is uncertain, we showed that recurrent aneurysms after an FDS could present with mass effects. Our treatment strategy involved placement of an additional FDS, which was feasible and resulted in complete obliteration of the aneurysm. Finally, the patient’s symptoms were relieved after treatment. We presumed that the reason for recurrence could be the size discrepancy between the proximal and distal ICA, putting aside the surgeon’s technique. For the initial treatment at the other hospital, a 5.0-mm sized FDS might have been selected due to the diameter of the proximal ICA, resulting in insufficient metal coverage in the neck.
Little is known about the efficacy and safety of retreatment when a giant aneurysm recurs. Incomplete obliteration and aneurysm volume changes after FDS treatment were more common than expected. In a previous study with a small number of cases, six out of eight large and giant aneurysms changed in size [3]. Additionally, potential risk factors of failed aneurysm occlusion after an FDS were found to be older patient age, prior stent implantation before an FDS, location in the distal anterior circulation, and longer follow-up duration [4]. The authors reported residual aneurysms in 16.4% of the patients, and 6.8% underwent retreatment. Another study reported residual aneurysms in 19% of patients and described fusiform shape, decreasing dome-to-neck ratio, and previous stent implantation as independent risk factors for treatment failure [15].
Patients are often symptomatic because of the mass effect of recurrent large or giant aneurysms. In cases where a patient has neurological symptoms correlated with recurrence of the aneurysm after an FDS, retreatment of the aneurysm should be considered. Because of the limited options for retreatment after an FDS, the predominant treatment strategy consisted of the placement of an additional FDS or parent artery occlusion. Goertz et al. reported the clinical and anatomical results of retreatment after initial FDS treatment with residual aneurysm perfusion. Their treatment strategy mainly consisted of the placement of additional FDSs. Complete occlusion of the parent artery, which can be performed in patients with sufficient collateral circulation, was not performed in any of the cases. This approach proved feasible and resulted in improved aneurysm occlusion in all the cases. At mid-term follow-up, the rates of complete and favorable aneurysm occlusion were 75.0% and 91.7%, respectively [6]. In the present case, the patient developed symptoms due to the mass effect of the aneurysm causing the bitemporal hemianopsia and the growth of the lateral ventricle, and retreatment was required for the aneurysm. The neurological symptoms improved after the recurrent aneurysm was treated with an additional FDS. In general, the symptoms caused by the mass effect of aneurysms are improved by endovascular treatment. Halbach et al. reported that symptoms due to mass effect disappeared completely after endovascular treatment in 50% of patients and gradually improved in 42.3% of patients [7].
FDS treatment is associated with higher morbidity and mortality rates than conventional coiling, and is mainly related to ischemic complications. These morbidity rates are not negligible and require careful consideration of the risks and benefits of the treatment. In this context, there is evidence that the complication rate correlates with the number of implanted FDSs [1]. Additionally, the use of multiple FDSs correlates with an increased risk of side vessel occlusion, which can, depending on the location, result in severe neurological deficits such as visual impairment or general ischemic complications [14]. Chalouhi et al. reported that complications occurred approximately three times more often with implantation of multiple FDSs (15%) than with a single FDS (5%). Therefore, the authors recommend minimizing the number of FDSs implanted. In another series, however, most aneurysms were initially treated with multiple stents due to complex morphology, large size, and/or insufficient immediate contrast stasis after placement of the first FDS. All patients received an additional FDS during retreatment. The authors did not observe any procedure-related morbidity [6]. In their series [6], side vessels arising from the parent artery were covered by the FDS in all but one patient; however, 76.9% of these vessels remained patent until the last follow-up. Two occlusions of covered side vessels were regarded as technical complications. However, the patients remained asymptomatic in both cases and there were no further technical or symptomatic complications during a cumulative follow-up period of 19.4 patient years, indicating that retreatment with FDSs when required is reasonably safe.
CONCLUSIONS
A giant aneurysm initially treated with the insertion of FDS and coils could be failed, resulting in aggravation of clinical symptom. Retreatment the recurred giant aneurysm with an additional FDS successfully relievd the aggravated symptom and achieved complete occlusion of the aneurysm. This case presents a potential feasible and safe treatment option for recurred giant aneurysms after treatment with an FDS.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
