Woven Endobridge (WEB) augmented by Y-stent in a shallow basilar tip aneurysm
Article information
Abstract
The Woven Endobridge (WEB) device can be an effective and simple treatment modality for wide-neck bifurcation intracranial aneurysms. We present a case of a shallow basilar tip aneurysm treated with the WEB device that required stabilization with Y-stent through radial access.
INTRODUCTION
The Woven Endobridge (WEB) is the only intrasaccular flow-disruption device that is approved by the United States Food and Drug Administration (FDA). As a standalone device, it has gained popularity for its efficacy and simplicity. While providers progress along their learning curve when attempting to use the WEB device, it is important to implement salvage techniques in the event of unfavorable anatomy or other technical complications.
CLINICAL PRESENTATION
A 71-years-old male with a history of chronic smoking, coronary artery disease, atrial fibrillation, and peripheral vascular disease had an unruptured basilar tip aneurysm. This was managed expectantly until surveillance imaging revealed enlargement. A diagnostic cerebral angiogram was then performed, and the patient was offered endovascular treatment with stent-assisted coiling or the WEB device. He elected to proceed with endovascular treatment, and was started on Aspirin and Plavix five days prior to the procedure.
TECHNIQUE
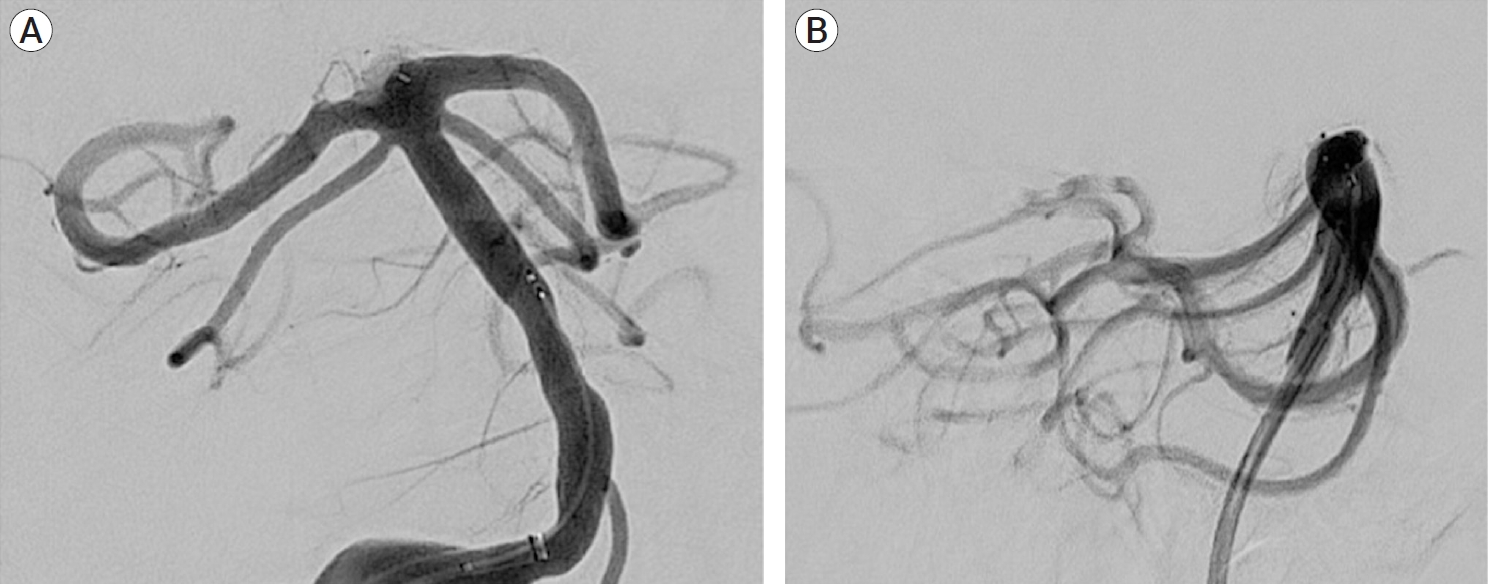
Under general anesthesia, the right radial artery was accessed with a micro-puncture kit and a 6-French sheath was placed. Radial access was chosen because it provided a short and direct access to the dominant right vertebral artery, as well as afforded a lower risk of access point hematoma since the patient was on dual antiplatelet therapy. A mixture of Verapamil and Nitroglycerin was injected through the radial sheath. A Bernstein Select catheter (Penumbra, Alameda, CA, USA) was advanced over a 0.035-inch Glidewire (Terumo, Somerset, NJ, USA) under fluoroscopy and the right vertebral artery was accessed. A road map was obtained and an exchange length Glidewire was introduced into the catheter. The catheter was removed leaving the exchange Glidewire in place. The sheath was removed and a 0.088-inch Neuron MAX catheter (Penumbra, Alameda, CA, USA) was advanced over the Glidewire into the vertebral artery. A new road map was obtained. The guide catheter was connected to a continuous-heparinized saline flush. Anterior-posterior, lateral, and three-dimensional images were obtained of the posterior circulation. The aneurysm measured 6.76×6.35×4.30 millimeters (mm) (Fig. 1), and a 7×3 mm WEB single-layer (SL) device (MicroVention-Terumo, Aliso Viejo, CA, USA) was selected. The patient then received 5000 units of Heparin, which was supplemented every 5-10 minutes to maintain the activated clotting time (ACT) between 250-300 seconds. A Synchro-2 microwire (Stryker Neurovascular, Fremont, CA, USA) inside a VIA catheter (MicroVention-Terumo, Aliso Viejo, CA, USA) inside a SOFIA EX catheter (MicroVention-Terumo, Aliso Viejo, CA, USA) were introduced as a triaxial support system into a guide. Under fluoroscopy, the Synchro-2 microwire and VIA catheter were advanced into the aneurysm. The SOFIA EX catheter was advanced to the mid-basilar segment for extra support. The WEB device was deployed and appeared to have good apposition in three corners, but was re-sheathed and then redeployed due to suspicion of leakage into the aneurysm. Conformation to the aneurysm neck was adequate, however complete occlusion was not achieved (Fig. 2). To maintain the WEB device in place and avoid risk of herniation after detachment, a 3.5×23 mm LVIS Junior stent (MicroVention-Terumo, Aliso Viejo, CA, USA) was deployed into the left posterior cerebral artery (PCA) down to the upper third of the basilar artery. This particular stent was chosen for the ease of tunneling into itself, in the event that Y-stent was needed. The first LVIS Junior stent conformed to the vessel and maintained the WEB device in place, but there was a small impingement of flow into the right PCA. The VIA catheter was advanced over a microwire through the left PCA stent and guided into the right PCA. Another 3.5×23 mm LVIS Junior stent (MicroVention-Terumo, Aliso Viejo, CA, USA) was deployed, resulting in a Y-shaped configuration (Fig. 3). Control runs were obtained which revealed adequate conformation and occlusion of the basilar artery aneurysm, with patency to remainder of posterior circulation (Fig. 4). All catheters and microwires were removed. Hemostasis was achieved at the wrist using TR Band (Terumo, Tokyo, Japan). The patient was extubated and recovered without complication.
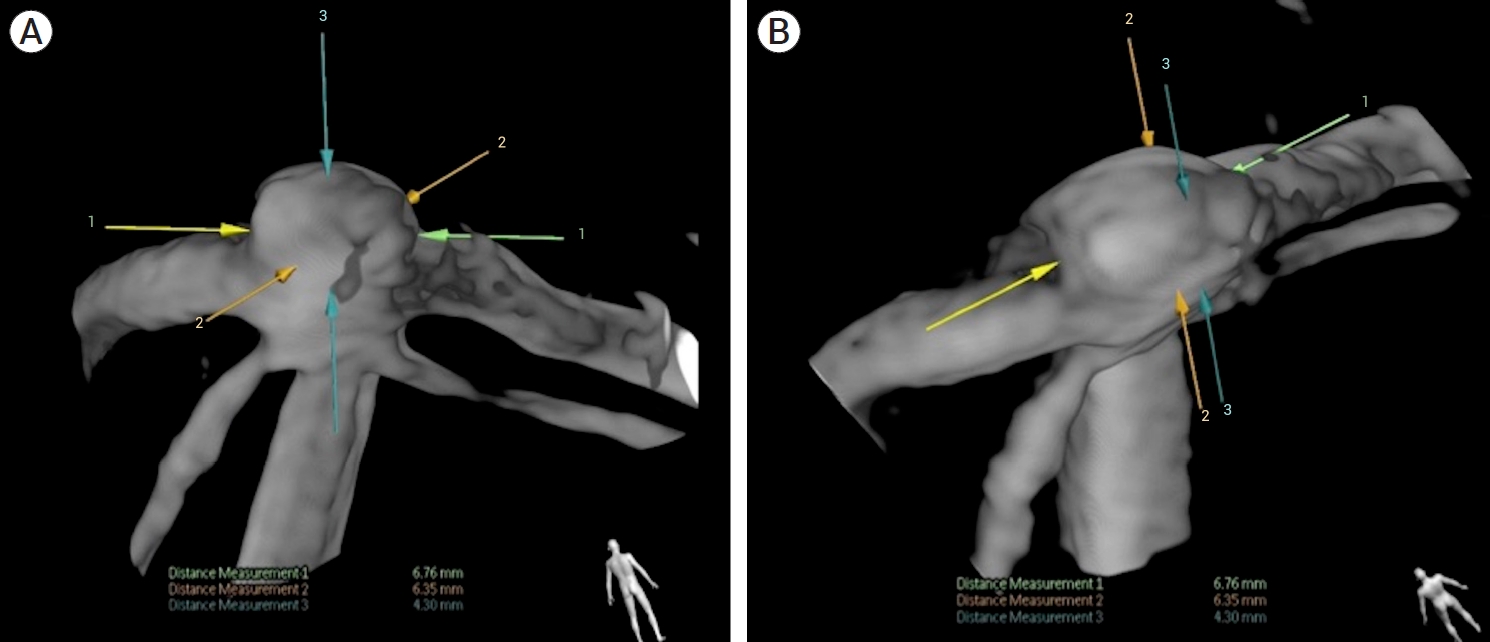
Three-dimensional (3D) reconstruction of basilar aneurysm in posterior (A) and left posterior oblique (B). Length 6.76 mm (arrows 1). Width 6.35 mm (arrows 2). Height 4.30 mm (arrows 3).

Deployment of Woven Endobridge (WEB) (MicroVention-Terumo, Aliso Viejo, CA, USA) into basilar tip aneurysm with conformational dimensions of 6.43 mm (L)×6.45 mm (W) (A) but inadequate occlusion (B).

Deployment of two 3.5×25 mm LVIS Junior stents (MicroVention-Terumo, Aliso Viejo, CA, USA) in Y-shaped fashion. First stent was deployed in the left posterior cerebral artery (A) and the second stent was placed into the right posterior cerebral artery (B).
DISCUSSION
Basilar tip aneurysms are frequently wide-necked [16], carry a higher risk of rupture [16], and continue to pose technical challenges in treatment. Endovascular coiling is commonly pursued [8], however limitations include low occlusion rate [14], recurrence and/or retreatment [1,14]. To address these downfalls, balloon remodeling [15], Y-stent-assisted coil embolization [2], and Waffle-cone stenting [10] have been implemented. Flow diversion is another option, however the proximity of small perforators and risk of occlusion limit their use [5]. Microsurgical clipping can also be performed but is complex and invasive.
The efficacy and safety profile of the WEB device for endovascular treatment of intracranial aneurysms has previously been investigated. Pierot et al. demonstrated one-year and two-year adequate occlusion rates of 79% [11] and 81% [12], respectively, and 94% occlusion rates in basilar bifurcation aneurysms [12]. The most common complication with the WEB device is thromboembolism (5-14%) [4,7,17], with middle cerebral artery (MCA) bifurcation aneurysms having a higher thromboembolic complication rate than posterior circulation aneurysms [7]. Recanalization and intraoperative rupture are less common, with a low incidence of device-related morbidity (0-1.3%) [4,9,11].
The literature pertaining to WEB plus Y-stent for basilar artery aneurysms is limited. Cagnazzo et al. reported treatment of 17 intracranial aneurysms using WEB plus stent, but all three basilar aneurysms required retreatment with Y-stent-assisted coiling due to inadequate occlusion [3]. Samaniego et al. describes two cases where WEB plus Y-stent was used to treat wide-necked basilar tip aneurysms [13]. One patient died from basilar artery occlusion and the other intervention was performed as a bailout maneuver but achieved great intrasaccular positioning of the WEB device [13]. Additionally, Lawson et al. reports one case where WEB plus stent achieved excellent results [6]. Our procedure also resulted in adequate occlusion without complications.
CONCLUSIONS
The advantage of using the WEB device is simplicity and avoidance of multi-device use. However, it is important to have salvage techniques available to either remove or stabilize the device to prevent migration and/or vessel occlusion. Generally, an incremental algorithm from simple to complex should guide treatment. In keeping with this principle, the authors intended to use a single WEB device for this aneurysm. This was preferred over stent-assisted coiling because it eliminated the need for long-term dual antiplatelet therapy. Unfortunately, the WEB device did not adequately conform to the shallow aneurysm. In order to minimize risk of WEB migration, the authors decided that placement of a stent would be needed to properly secure it in place. Whereas a single stent would have been preferable, Y-stent was needed to preserve the patency of both PCAs and ensure adequate occlusion in this basilar tip aneurysm. .
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.