Y-configuration Stent-assisted Coil Embolization for Wide-necked Intracranial Bifurcation Aneurysms
Article information
Abstract
Objective
The objective of this study was to determine the efficiency and safety of Y configuration stent-assisted coiling with double-closed stents for wide-necked intracranial aneurysms located at arterial bifurcations thorough analysis of a multicenter case series.
Materials and Methods
A retrospective chart review was done on 10 patients who underwent endovascular treatment of wide-necked intracranial aneurysms with Y-configuration stent-assisted coil embolization in three centers from August 2011 to March 2014. The degree of aneurysmal occlusion was assessed using the Raymond scale. Clinical outcomes were assessed before operation, at discharge, and at the last follow-up visit using the Glasgow outcome scale.
Results
The 10 patients included 6 females and 4 males with a mean age of 58.6 years. Indications for treatment included 6 unruptured intracranial aneurysms and 4 ruptured intracranial aneurysms. Five aneurysms were located at the basilar artery bifurcation, four aneurysms were located in an anterior communicating artery, and one aneurysm was in the pericallosal artery. The mean size of the 10 aneurysms was 9.7 mm. All aneurysms had a dome-to-neck ratio of < 1.5 (mean, 0.89). Immediate complications included one thromboembolic event out of the 10 cases. Immediate posttreatment angiograms showed complete occlusion in 1 aneurysm and residual necks in 9 aneurysms. Follow-up results showed 8 complete occlusions and 2 residual necks. No delayed complications were observed during the follow-up period (mean: 20 months).
Conclusion
Y configuration using double-closed cell stents is feasible and safe in selected patients. This method is an acceptable option for managing complex wide-necked bifurcations.
INTRODUCTION
Endovascular treatment has been increasingly used for intracranial aneurysms in the past decade. Since the International Symptomatic Aneurysm Trial was published, endovascular treatment of intracranial aneurysms has become the first treatment option in many centers.17) Recent advances in endovascular techniques and devices such as stent-assisted coiling, balloon remodeling, neck bridges, waffle cones, and so on have allowed treatment of more challenging aneurysms, such as wide-necked or complex aneurysms.13)16)18)20) However, wide-necked intracranial aneurysms in arterial bifurcations that are treated by single stent still remain challenging owing to the difficulty in holding the coils inside the aneurysm sac and the high risk of recanalization.9)10) A double-stent technique in the Y configuration was first introduced by Chow et al. in 2004.8) Since then, many reports have demonstrated low morbidity and mortality rates associated with Y-stenting.11)30) These reports dealt with open-open or open-closed stent combinations.11)28) Herein, we report the efficacy and safety of Y configuration stent-assisted coiling with closed-closed stents for wide-necked intracranial aneurysms located at arterial bifurcations. We also perform a literature review.
MATERIALS AND METHODS
Three centers provided retrospective data for all consecutive patients with intracranial aneurysms treated with Y configuration-assisted stents using close-cell stents (Enterprise, Codman, Raynham, MA, USA). Each center provided clinical, procedural, and angiographic data for each patient.
Patients and aneurysms
A retrospective chart review was conducted for all patients who underwent endovascular treatment of aneurysms with Y configuration-assisted stents in three centers from August 2011 to March 2014. Patients for whom preprocedural evaluation was done using a stent-assisted coiling technique in the Y-stent configuration were included. Patients for whom an open-cell type stent was used for preprocedural evaluation were excluded from the analysis. All aneurysms were wide-necked and located in an arterial bifurcation of basilar artery, anterior communicating artery or pericallosal artery. Aneurysms were classified as small (2-6 mm), medium (7-12 mm), large (13-24 mm), and giant (≥ 25 mm). Wide-necked aneurysms were defined as having a large neck (> 4 mm) and/or a dome-to-neck ratio of < 2.
Endovascular procedures
All endovascular procedures were performed with patients under general anesthesia. Patients with unruptured aneurysms were treated with a daily dual antiplatelet drug regimen consisting of clopidogel (75 mg) and aspirin (100 mg) for at least 5 days. Platelet-aggregation inhibition was tested in all patients with unruptured aneurysms (VerifyNow P2Y12 assay) one day before the procedure. Further loading doses of aspirin and/or clopidogrel were administrated when necessary. During the procedure, a bolus injection of 3,000 IU heparin was given and a further 1,000 IU of heparin was administered per hour. Anticoagulation levels were monitored to maintain an activated clotting time 2-3 times of the baseline value. Patients with acutely ruptured aneurysms were treated with intravenous tirofiban soon after stents were deployed without heparinization. Heparin was discontinued after the procedure. All procedures were performed via a unilateral or bilateral transfemoral approach. Coiling was performed before and after delivery of stents.
For the Y-stent configuration technique, a 6F or 7F guiding catheter was first navigated into the distal internal carotid artery for anterior circulation aneurysms or the distal vertebral artery for posterior circulation aneurysms. After angiographic images were acquired in the anteroposterior, lateral, working, and 3D rotational views, the sequence of stent placement was determined. Before deployment of the first stent, the aneurysm was catheterized with a microcatheter and microwire. An Enterprise transport microcatheter (Prowler Select Plus, Codman, Miami Lakes, FL, USA) was placed at the aneurysm neck and the distal tip of the transport microcatheter was placed in the efferent artery. After positioning, the Enterprise stent was slowly inserted through the transport microcatheter. The first stent was placed in the most acutely angled branch. The second stent was navigated through the stent cell of the first stent into the contralateral branch vessel and proximal half while overlapping with the first stent. In case of need to flow diversion, stents was deployed in a parallel fashion from each other distal artery to the proximal artery, forming a kissing Y configuration. Aneurysms were then occluded with a variety of available coils. Femoral puncture sites were closed with closure devices. Following the procedure, dual antiplatelet drugs were administered. In all patients, clopidogrel was stopped after 6 or 12 months. Aspirin was continued indefinitely.
Occlusion grade
The degree of aneurysmal occlusion was assessed using the Raymond scale,21) and was classified into complete occlusion, residual neck, and residual aneurysm.
Clinical outcomes and angiographic follow-up
Clinical outcomes were assessed before operation, at discharge, and at the last follow-up visit using the Glasgow outcome scale (GOS). A good outcome was defined as a GOS score of 4-5. A poor outcome was defined as a GOS score of 0-3.
Angiographic images were obtained in the anteroposterior, lateral, and working projections before treatment and immediately after treatment. The imaging follow-up modalities used were conventional angiography and magnetic resonance (MR) angiography. 3 patients underwent conventional angiography only if they agreed to do so. Angiographic follow-up was done 12-24 months after endovascular treatment. The Raymond scale (total occlusion, residual neck, and residual aneurysm) was used to assess the results of the procedure.
RESULTS
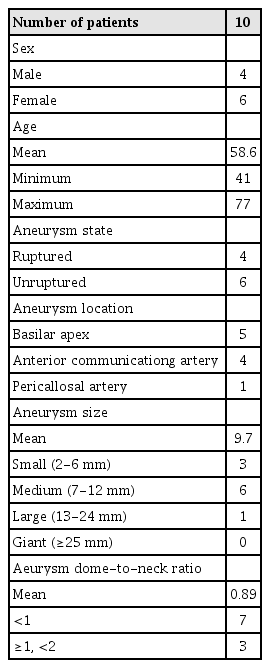
A total of 10 patients underwent treatment with closed cell type Y configuration stents for 10 wide-necked bifurcation cerebral aneurysms at the three participating centers from 2011 to 2014. Data on patients and aneurysms are summarized in Table 1. The patients included 6 females and 4 males with a mean age of 58.6 years (range, 41-77 years). Indications for treatment included 6 unruptured aneurysms and 4 ruptured aneurysms. All aneurysms were wide-necked at a bifurcation, including 5 aneurysms located at the basilar artery bifurcation, 4 aneurysms in the anterior communicating artery, and 1 aneurysm in the pericallosal artery (Fig. 1). Of the 10 aneurysms (mean 9.7 mm, range 5-12 mm), one was large, six were medium, and the remaining 3 were small in size. All aneurysms had a dome-to-neck ratio of < 1.5 (mean ratio, 0.89, range: 0.65-1.13).

A 44-year-old woman with an unruptured pericallosal bifurcation aneurysm. (A) 3D rotational reconstruction image produced by cerebral angiography showing an approximately 5 mm sized wide-necked basilar bifurcation aneurysm. (B) A completely occluded necked aneurysm after a Y configuration-assisted double stent procedure using closed cell-type stents. (C) Complete occlusion of the aneurysm on follow-up conventional angiography performed after 23 months.
Immediate complications included one thromboembolic event out of the 10 cases. A 45-year-old female was admitted for endovascular treatment of an unruptured aneurysm located in the anterior communicating artery. The aneurysm was incidentally found on MR angiography performed for dizziness. On conventional angiography, the aneurysm was wide-necked (11.3 mm in size) with a 1.12 dome-to-neck ratio. The 7F guidance catheter was placed in the right proximal internal carotid artery. The microcatheter (Excelsior SL-10, Stryker, Fremont, CA, USA) was inserted into the aneurysm sac with a microwire (Synchro-14, Stryker, Fremont, CA, USA). The transport microcatheter was navigated into the left distal A2. After the first coil was inserted into the aneurysm, deployment of closed-cell stent was done from left A2 to left A1. Thrombus formation in the stent was encountered. The in-stent thrombosis was completely resolved with intra-arterial infusion of 100,000 IU Urokinase and 200 mcg Tirofiban. The transport microcatheter was navigated into the other distal A2 segment through the stent cell of the initial stent. Coiling was completed and occlusion was satisfactory. However, the patient experienced mental deterioration the next day. We found recurrent in-stent thrombus formation in the same area and performed thrombolysis. Infarctions in the bilateral fornix and corpus callosum genu body were evident on magnetic resonance angiography. The patient was discharged with mild short-term memory impairment. Successful Y-configuration stent-assisted coil embolization was achieved for all 10 aneurysms. One aneurysm of basilar apex was performed by kissing Y configuration, because it needed to flow diversion.
An immediate posttreatment angiogram showed complete occlusion in 1 aneurysm and a residual neck in 9 aneurysms. In the follow-up period, 3 patients underwent conventional angiography, whereas the others underwent MR angiography. Follow-up results of the 10 aneurysms showed 8 complete occlusions and 2 residual necks. Post-operative follow-up angiograms were obtained at a mean of 17.10 months. The two aneurysms with residual necks were both located in the basilar artery bifurcation. Overall, the 9 patients had a GOS score of 5 and only one patient at discharge. No delayed complications were found at follow-up (mean, 20.20 months, range: 13-43 months). Patient data are summarized in Table 2.
DISCUSSION
Coil embolization is a standard treatment for cerebral aneurysms. Advances in endovascular techniques have allowed more challenging aneurysms to be treated with coil embolization. The advent of self-expanding stents has greatly improved the ability to treat intracranial aneurysms. Stent deployment offers mechanical support to prevent coil prolapse or migration. Additionally, stent-assisted coil embolization has allowed increased packing density with enhanced endothelialization.5) Despite the introduction of a variety of techniques, such as balloon remodeling,3) the waffle-cone technique,13) and so on, wide-necked and complex aneurysms are still challenging even when a single stent is deployed. In 2004, Chow et al.8) first described double open-cell Neuroform (Boston Scientific, Fremont, CA, USA) stents in a Y configuration. Because an open-cell stent can allow for easier passing of the other stent, Y configuration stent-assisted coil embolization using open-cell stents is technically feasible. Nevertheless, Neuroform stents present difficulties in passing tortuous vessels. The transport microcatheters of Enterprise stents are more flexible and navigable than are Neuroform stents.29) Therefore, we used Enterprise stents in the current study.
The Y configuration stent-assisted technique was originally used in the peripheral vasculature to treat bifurcations.26) This technique was applied to treat intracranial aneurysms. Y configuration stent-assisted technique using two open cell-type stents was first performed because open cell-type stents allow for relatively easy passage through the stent cells of the deployed stent. However, open cell stents may cause migration of the initial stent during deployment of the second stent.15) In our cases, Y-configuration stent-assisted coil embolization was performed using closed cell-type stents in all cases without any technical difficulties. The problem that we encountered involved navigation of the microcatheter in the acutely angled branch for deployment of the first stent. When it was difficult to pass the acutely angled branch, we accessed the distal artery with an SL-10 microcatheter (Excelsior SL-10, Stryker, Fremont, CA, USA) and changed the transport microcatheter. Enterprise stents have anchoring flared ends, making stent deployment easier. They reduce the risk of stent migration during the passage of the microcatheter for deployment of the second stent. Y-configuration stent-assisted coil embolization using two closed-type stents is technically feasible.
Several concerns about the use of two closed cell-type Y stents were raised. First, the closed cell-type stent is technically more difficult to navigate through stent cells than open cell-type stent. However, other reports have demonstrated a success rate of approximately 100%, except in 1 case.1)7)23) In our study, all cases of Y-stenting were successful completed. The first stent was more difficult to deploy because of the acutely angled branch. Second, the Y-stent technique using double closed cell stents may cause narrowing of the second stent because of the small stent cells of the initial stent. A floating stent can be a source of thrombosis. It may impair antegrade blood flow. Fargen et al. reported an incidence of in-stent stenosis in Y-stent-assisted coiling in a large multicenter retrospective study.11) In-stent stenosis < 50% was seen in 5 of 30 (17%) patients upon angiographic follow-up. However, none of those patients required treatment for stenosis.11) There was no case of in-stent stenosis treated with closed cell-type stents. In addition, the percentage of delayed thromboembolic events was only 3.1%.11) In our study, in-stent stenosis or delayed complications at follow-up were not found. Only one case of in-stent thrombus formation was experienced during the procedure.
The most important advantage of Y configuration stent-assisted coiling is that it can prevent coil prolapse and occlusion of a branching artery by allowing for adequate vascular reconstruction of the parent artery and distal branch artery. Use of a single stent carries a risk of occlusion branch artery and coil prolapse at arterial bifurcations. The other advantage of Y configuration stents is that they have an effect on flow diversion. Post-procedural hemodynamic alteration is likely to be an important factor in determining the long-term morbidity and mortality of endovascular intervention.4) In 2009, Tateshima et al. demonstrated significant alteration of flow direction, velocity, and pattern before and after stent placement in a silicone aneurysm model.27) In another in vitro study, Rhee et al. reported that stent placement can reduce the magnitude and pulsatility of the wall shear rate.22) Y configuration stent placement reduces cross-neck flow in computational fluid dynamic simulations of wide-necked aneurysms and shear stresses inside the aneurysm sac by > 40% at the end of the cardiac cycle.2)6) In another in vitro study using a silicone block model of a bifurcation, K. Kono and Terada demonstrated that the cycle-averaged velocity and wall shear stress in an aneurysm are reduced by 48-54% when using closed cell-type Y configuration stents.14) Some procedures resulted in complete occlusion or a reduction in filling of aneurysms without additional coiling by using closed cell-type Y configuration stents.7)
In the current study, the initial immediate angiographic occlusion rate was 1 complete occlusion and 9 residual necks out of the 10 cases. Upon angiographic follow-up, we observed improvement in 7 aneurysms and stability of 2 aneurysms. Although 9 aneurysms displayed small residual filling upon initial treatment, 7 aneurysms were developed spontaneous thrombosis on angiographic follow-up. Spiotta et al. reported similar results.25) Spontaneous thrombosis in the aneurysmal sac could be due to the effect of flow diversion when using closed cell stents.
Aneurysm recurrence is a disadvantage of coil embolization compared to surgical clipping. A literature search revealed a recanalization rate of 14% after single stent-assisted coiling.24) With conventional coiling, the recanalization rate is reported to be 20% and 35.3% for wide-neck small aneurysms and large aneurysms, retrospectively.19) Aneurysms with a neck width greater than 4 mm and a maximum diameter greater than 10 mm carry a three-fold higher risk of recurrence following treatment.12) Yavuz et al. reported that the recanalization rate was only 2.2% (4 recanalizations/186 follow-up aneurysms) in 193 aneurysms treated by Y configuration stent-assisted coiling.30) In the current study, no recanalization occurred. Therefore, retreatment was not necessary. This result could be due to the fact that Y configuration-assisted double stents using closed cell type stents may affect flow diversion.
This study has several limitations. It was a retrospective study on a small number of cases. In addition, patient selection bias might have occurred. Furthermore, the follow-up time was relatively short.
CONCLUSION
Wide-necked bifurcation aneurysm is challenging for neuro-interventionists. Y configuration stenting using double closed cell stent-assisted coiling is feasible and safe for selected patients in the management of complex wide-necked bifurcations. However, further study using this technique in a prospective study with a large population and a long follow-up period is merited.