Multiple Intracranial Aneurysms Associated with Behçet's Disease
Article information
Abstract
Behçet's disease is an inflammatory disorder involving multiple organs. Its cause is still unknown, but vasculitis is the major pathologic characteristic. The common vascular lesions associated with Behçet's disease are aneurysm formation, arterial or venous occlusive diseases, and varices. Arterial aneurysms mostly occur in large arteries. Intracranial aneurysms hardly occur with Behçet's disease.
We would like to present a 41-year-old female patient with Behçet's disease who showed symptoms of severe headache due to subarachnoid hemorrhage. Brain computed tomography revealed multiple aneurysms. We also present a literature review of intracranial arterial aneurysms associated with Behçet's disease.
INTRODUCTION
Behçet's disease is a multisystem inflammatory disorder characterized by recurrent oral and genital ulcers and uveitis. Although the medical understanding of this disease has advanced, its origin remains unknown.14)15) The vasculitis shown in Behçet's disease is the major pathologic characteristic, due to the involvement of both arteries and veins of all sizes.4) The common vascular lesions associated with Behçet's disease are aneurysm formation, arterial or venous occlusive diseases, and varices17). Aneurysms mostly gets developed in the abdominal aorta, femoral arteries, and pulmonary arteries. Intracranial aneurysms are very rare lesions in Behçet's disease.2)3)6)7)9)10)11)13)16)17)
In this study, we present the case of a patient with multiple intracranial aneurysms. We also include a broad review of the literature about Behçet's disease-associated intracranial aneurysms.
CASE REPORT
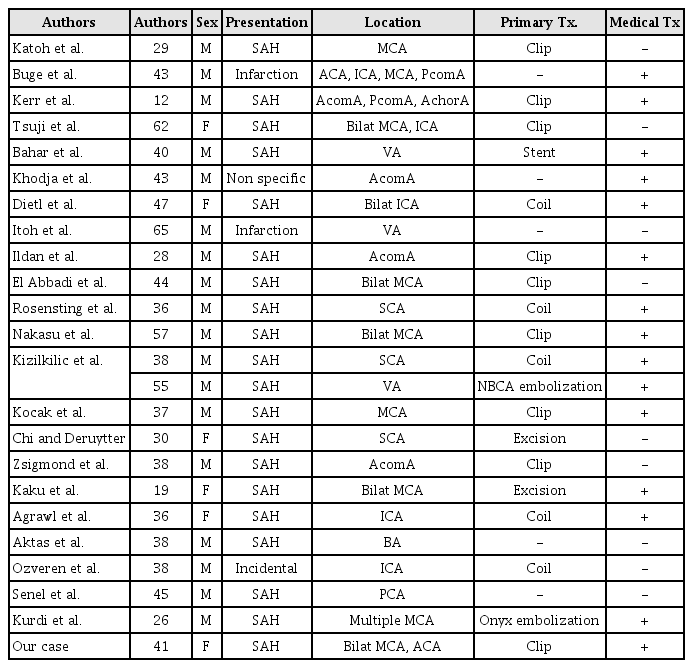
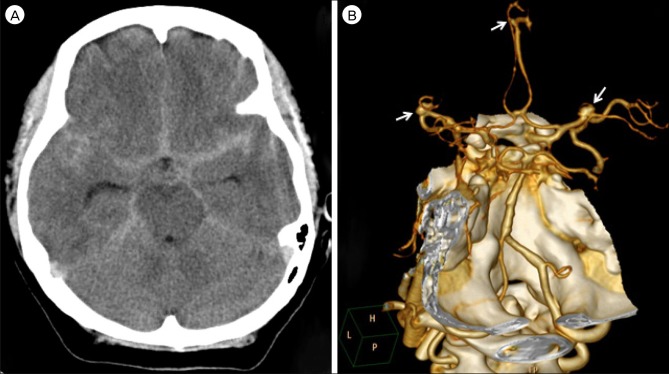
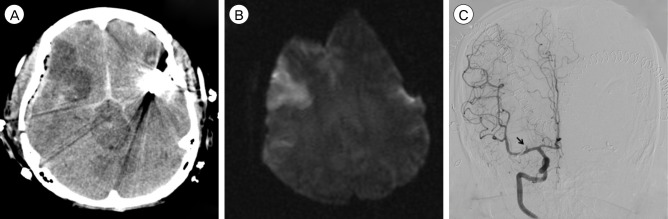
A 41-year-old female patient was admitted to our institute owing to the sudden onset of severe headache. According to her medical history, she had been diagnosed with Behçet's disease about three years ago, but have not received any specific treatment. When admitted, she was neurologically intact, except for the headache and the routine blood test showed nothing specific. Prompt brain computed tomography (CT) with angiography was performed and it showed diffuse subarachnoid hemorrhage (SAH) in the basal cistern (Fig. 1A) and multiple aneurysms in both the middle cerebral arteries (MCA) and the anterior cerebral artery (ACA) (Fig. 1B). The ACA aneurysm was considered unlikely to be the source of the rupture, due to its small size because both MCA aneurysms were very similar in their shapes, sizes, and locations, we could not clearly determine which aneurysm had ruptured. Therefore, we decided to clip both MCA aneurysms at once and treat the small ACA aneurysm with steroids (prednisolone 125 mg, 3 times a day) in accordance with Nakasu et al.11) who reported the effectiveness of steroids to the small aneurysm associated with Behçet's disease. Intraoperative findings revealed that the left MCA aneurysm was ruptured. There were no specific findings in either MCA at surgery. The patient was treated with triple H (3H) therapy postoperatively and admitted to the neurologic intensive care unit. At the second day postoperation, routine follow-up CT showed a low-density lesion in the right (Rt.) MCA territory (Fig. 2A). Brain magnetic resonance imaging performed immediately showed acute infarction in the same area (Fig. 2B). However, there were no specific symptoms or signs associated with this radiologic finding. The echocardiogram was normal. On the Rt. internal carotid artery (ICA) angiogram, obstruction of the Rt. M1 branch was seen (Fig. 2C). We performed chemical angioplasty with Nimotop 10 mg over 20 minutes and began anti-platelet medications (aspirin 100 mg and Pletal 200 mg per day). There were no other specific events during her hospital stay in any other respects. After 24 days of hospitalization, she was discharged without any neurologic sequelae. At the 20th day after discharge, CT angiography was performed in the outpatient department that showed revascularization of the previously obstructed Rt.M1 branch (Fig. 3A) and the persistent ACA aneurysm. The most recent follow-up CT performed 3 years after the initial examination showed no regrowth of the previously clipped aneurysms. However, the ACA aneurysm was still presented without any changes in size, shape, etc. despite continuous steroid therapy (Fig. 3B).
(A) A CT scan obtained on admission showing a diffuse SAH in the basal cistern. (B) A 3D reconstructed CTA showing multiple aneurysms at both MCAs and ACA (arrow). CT = computed tomography; CTA = CT angiography; SAH = subarachnoid hemorrhage; MCA = middle cerebral artery; ACA = anterior cerebral artery.
(A) A CT obtained on the 2nd day postoperation showinga low-density lesion in Rt. MCA territory. (B) Diffusion-weighted imagerevealingrestricted diffusion in the same area. (C) A Rt. ICA angiogram showing obstruction of Rt. M1 branch (arrow). CT = computer tomography; MCA = middle cerebral artery; ICA = internal carotid artery.
3. (A) A CTA on the 20th day after discharge showing the revascularization of the previously obstructed Rt. M1 branch and the persistent ACA aneurysm (arrow). (B) A CTA performed 3 years after the initial exam showing ACA aneurysm without any changes in size or shape despite continuous steroid therapy. CTA = CT angiography; ACA = anterior cerebral artery.
DISCUSSION
Behçet's disease is a multisystem inflammatory disorder. According to the International Study Group guidelines, for a patient to be diagnosed with Behçet's disease, the patient must have oral ulcers along with 2 out of the following 4 "hallmark symptoms"; genital ulcers, skin lesions, eye inflammation, pathergy reaction.5)
There have been many theories about the origin of this disease, including a possible viral etiology, bacterial infection, autoimmune mechanisms, immunological factors and genetic predisposition. Although the medical understanding of this disease has been advanced, its cause is still unknown.14)15)
Neuro-Behçet's disease, involving the central nervous system, is found in approximately 10-25% of patients with Behçet's disease. The neurologic symptoms and signs begin most commonly after four to six years from the diagnosis of Behçet's disease, which may include headache, vomiting, motor and sensory disturbance, cerebellar and extrapyramidal signs, dementia, emotional instability, etc.15) The most common pathologic findings are focal necrotic lesions with infiltration of lymphocytes around small vessels, microcystic softening, demyelination, and gliosis. Lesions are commonly located in the brainstem and basal ganglia.15)
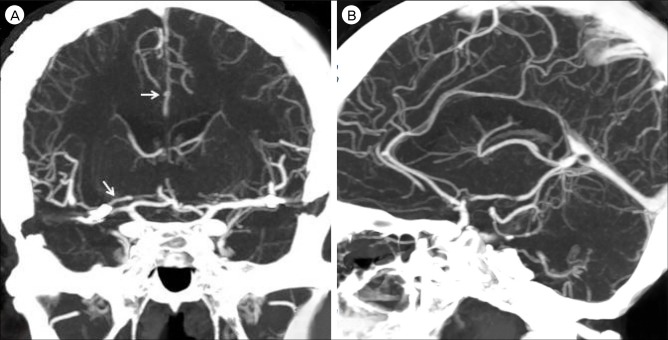
Vascular involvement may occur in 7-29% of patients with Behçet's disease. The common vascular lesions associated with Behçet's disease are aneurysm formation, arterial or venous occlusive diseases, and varices.12) Aneurysms mostly gets developed in the abdominal aorta and femoral and pulmonary arteries. Extracranial aneurysm formation in Behçet's disease is well known, but intracranial aneurysms with Behçet's disease are rare. So far, 23 cases of intracranial intracranial aneurysms in Behçet's disease were reported in the papers. All 24 cases, in addition to our case, were summarized in Table 1.2)3)6)7)9)10)11)13)16)17)
The histopathologic findings of aneurysms comprise ruptured internal and external elastic laminae with thickening of the tunica media, and vasculitis of the vasa vasorum with perivascular lymphocytic infiltration.15) However, there were no histologic findings of vasculitis in the two cases with cerebral aneurysms reported by Katoh et al. and Tsuji et al.6)16) In this respect, the correlation between Behçet's disease and cerebral aneurysms may be coincidental. Nevertheless, the relatively high incidence rate of multiple aneurysms in Behçet's disease may suggest the possibility that Behçet's disease has some function in the formation of cerebral aneurysms.11)
In the treatment of cerebral aneurysms in Behçet's disease, the location, size, and state (ruptured or not) of the aneurysm should be considered.13)
Surgical treatment is the first choice in cases of ruptured aneurysm.9)11) Endovascular treatment could be an option for ruptured aneurysms. However, insertion of the arterial catheter may cause either a thrombosis or pseudoaneurysm formation at the puncture site in patients with Behçet's disease.8) The risk of rebleeding may also be increased, if there is a vasculitis associated with Behçet's disease.1)
Unlike non-Behçet's disease aneurysms, medical treatment could be used in Behçet's disease-related unruptured aneurysms. Nakasu et al.11) reported the disappearance of an unruptured cerebral aneurysm after steroid therapy. Zelenski et al.17) also reported the effectiveness of cytotoxic agents and steroid therapy. However, Kerr et al.7) reported a bad outcome of steroid therapy for a ruptured aneurysm with SAH. This is probably due to steroid-resistant disease due to prolonged steroid therapy.11) Interestingly, the unruptured, small ACA aneurysm in our case did not disappear or change at all despite steroid therapy and no history of previous steroid therapy. To our knowledge, this ineffectiveness of steroid treatment without any history of steroid therapy has not been previously reported in the literature at all. Although the mechanism and effects of steroids remains unclear, medical treatment is considered as the first choice in unruptured cases, but serial close follow up is needed to check the outcome of the treatment.
CONCLUSION
Behçet's disease with intracranial aneurysm is rarely found, but continues to be reported. We should not underestimate this critical disease, and proper choice of treatment is necessary for the safe and effective management of intracranial aneurysms in Behçet's disease.
Notes
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.