Fusiform Superior Cerebellar Artery Aneurysm Treated with Endovascular Treatment
Article information
Abstract
An aneurysm of the distal superior cerebellar artery (SCA) is a highly rare disease. Fusiform aneurysms of the distal SCA are particularly challenging to treat. Clipping, trapping with or without bypass using microsurgery or endovascular treatment (EVT) were used to treat this condition. We describe the case of fusiform distal SCA aneurysms treated successfully with endovascular coiling with a 3-month follow-up. A 39 year-old male was presented with subarachnoid hemorrhage (SAH) and a 15 mm fusiform aneurysm of the ambient segment of the left distal SCA. EVT for parent artery occlusion and packing of the aneurysm was done. Left sixth nerve palsy appeared after 1 day of EVT. The symptom completely recovered within 1 week of the post-procedural period. No neurological deficit was seen during the clinical 3-month follow-up. EVT of fusiform distal SCA aneurysms with coils is a safe and feasible option to manage this rare condition. However, the treatment options must be carefully selected depending on the neurologic condition, development of collateral circulation, and configuration of the dissection.
INTRODUCTION
Aneurysms of the distal superior cerebellar artery (SCA) are very rare and account for less than 0.2% of all treated intracranial aneurysms.1) Fusiform aneurysms of the distal SCA are particularly challenging to treat. Clipping, trapping with or without bypass using microsurgery or endovascular surgery were used to treat this condition. We describe the case of fusiform SCA aneurysms treated successfully with endovascular coiling with 3-month follow-up.
CASE REPORT
A 39 year-old male without past notable medical history was admitted with a sudden headache and neck stiffness. Brain computed tomography (CT) demonstrated evidence of Fisher Grade III subarachnoid hemorrhage (SAH) predominance of the pre-pontine, left ambient and quadrigeminal cistern (Fig. 1A), and a fusiform aneurysm of a left distal SCA was revealed on the CT angiography (Fig. 1B). Subsequent digital subtraction angiography (DSA) revealed the fusiform dilatation (12 mm length; 4.5 mm width) involving the ambient segment of the left distal SCA. The left SCA was duplicated ahead of the aneurysm and there was sufficient collateral circulation from the ipsilateral anterior inferior cerebellar artery (AICA) and posterior inferior cerebellar artery (PICA) (Fig. 2). The aneurysm was treated by endovascular occlusion of the aneurysm sac and the involved branch. Under general anesthesia an Excelsior SL-10 microcatheter was used to access the aneurysm. Seven detachable platinum coils were used to obliterate the lesion. Post-procedural angiography showed complete occlusion of the aneurysm sac and involved the SCA branch (Fig. 3). There was no immediate complication after embolization. Diffusion MRI was done 8 hours after embolization. MRI revealed scattered high signal change on the left posterior tegmentum, superior vermis, and superior part of the left cerebellum (Fig. 4). Left sixth nerve palsy occurred in the patient 1 day after EVT. The symptom completely recovered within 1 week of the post-procedural period. No neurological deficit was seen during the clinical 3-month follow-up.
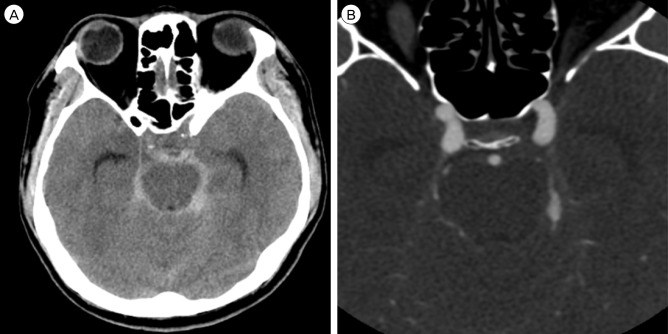
(A) Brain computed tomography (CT) image. The brain CT shows a Fisher Grade III SAH in the pre-pontine, left ambient and quadrigeminal cistern. (B) Brain computed tomography angiography (CT angiography) image. The brain CT angiography shows fusiform dilatation of the left distal SCA. SAH = subarachnoid hemorrhage; SCA = superior cerebellar artery.
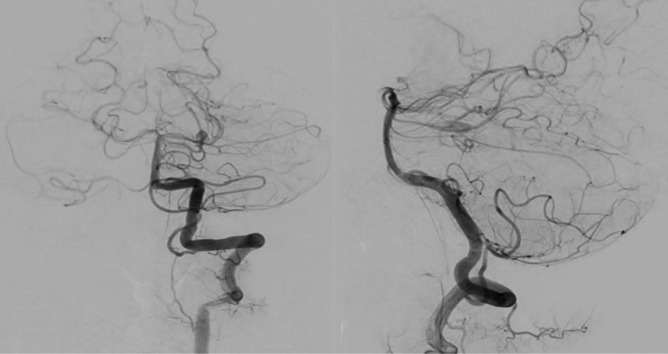
Digital subtraction angiography (DSA) images. The DSA images show the fusiform aneurysm of the left superior cerebellar artery. There was sufficient collateral circulation from the ipsilateral AICA and PICA. AICA = anterior inferior cerebellar artery; PICA = posterior inferior cerebellar artery.

Pre-operative 3-dimensional (D) CT angiography (left) and post-operative 3D DSA images (right). The 3D CT angiography reveals fusiform dilatation of the left distal SCA (left). The 3D DSA shows complete occlusion of the aneurysm sac and involved the distal SCA branch. The ipsilateral duplicated SCA is intact. CT = computed tomography; DSA = digital subtraction angiography; SCA = superior cerebellar artery.
DISCUSSION
Non-saccular aneurysms are often referred to as fusiform, dissecting, or trunkal aneurysms.2) According to some authors, the majority of these spontaneous, non-saccular aneurysms originate from vessel dissection.4)5)6) Fusiform aneurysms of the distal SCA are extremely rare and only 17 cases are reported in the literature. SAH was the most common clinical presentation.11) However, some reported cases were also presented with ischemic events.7) Most of the aneurysms in the distal SCA usually present with SAH. A hematoma predominantly in the pre-pontine cistern should raise suspicion of the probability of an SCA aneurysm. The exact rate of re-bleeding is not known but re-bleeding has been reported in the literature. Due to re-bleeding risk, DSA for accurate evaluation of a distal SCA aneurysm and early treatment in the acute phase is recommended in some studies.3)5)
The fusiform aneurysms of the distal SCA are particularly challenging to treat. First, surgical treatments of these aneurysms were suggested such as parent artery occlusion, clipping of the aneurysm body, trapping with or without bypass, and wrapping.9) These surgical treatments are associated with good results, however, an invasive approach should be considered for clipping or trapping of aneurysms and injury of cranial nerves III and IV, originating from the brain stem adjacent to the SCA. Second, EVT for embolization of the sac or parent arteries with platinum coils or other embolic materials is suggested as a good therapeutic option to treat these aneurysms. These techniques were used in recently reported cases with favorable results.1)4)5)9) Maintenance of the parent vessel patency is an important issue associated with these procedures as flow preservation demands more risky and complex techniques.
In our case, the SCA was duplicated ahead of the aneurysm and collateral circulation of the cerebellum from the AICA and PICA was sufficient. We selected EVT treatment of the distal SCA aneurysm, regardless of bypass surgery. The distal SCA is frequently duplicated. Furthermore, good collaterals can exist between the SCA and both the AICA and PICA through the vermian arcade and also with the paramedian branches and perforators of the basilar artery.8)10) If a patent artery with total SCA occlusion is necessary, these collateral circulations must be considered. However, in the current case, acute infarction in the SCA territory after EVT of total occlusion and sixth nerve palsy complication occurred 1 day after the procedure. Evaluation of collateral circulation and possibility of bypass surgery should be considered for total occlusion of the distal SCA that includes the aneurysm sac by EVT.
CONCLUSION
A fusiform distal SCA aneurysm is rare and present with infarction or SAH by rupture of the aneurysm. Surgical treatment must consider the anatomical structure, brain swelling, and technical challenge of a bypass. In this instance, parent artery total occlusion by EVT can be a feasible treatment option. However, a pre-operative evaluation, including the location of the aneurysm, presence of duplicated SCA, and sufficient collateral circulation should be carefully considered to minimize regional infarction.
Notes
Poster, the 55rd Annual Meeting of the Korean Neurosurgical Society, republic of Korea, October 15-18, 2015.
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.

