 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 18(3); 2016 > Article |
|
Abstract
Objective
Endovascular treatment is one of the most important treatments along with open craniotomy for cerebrovascular surgery. The successful treatment of endovascular disease relies on appropriate instruments and the surgeon's skill. Endovascular treatment needs to provide safe and stable access to the catheter cavity. Additionally, it is important to maintain a round shape without changing to an oval shape. The catheter for endovascular treatment has to be flexible and accommodate at least 0.027 inches of inner diameter. The 6-Fr NavienŌäó Intracranial Support Catheter (formerly the ReFlex Intracranial Catheter; Covidien Vascular Therapies, Mansfield, MA, USA) provides 0.072 inches of inner diameter.
Materials and Methods
We reviewed 61 cases for 56 cases of endovascular treatment with a Navien catheter. A triaxial system was used for all procedures with femoral arterial access. The Navien catheter was placed in the petrous segment of the internal carotid artery or third segment of the vertebral artery. The patients had various shapes of intracranial arteries, including tortuous vessels.
Results
The Navien catheter was used for 61 cases of endovascular treatment. We had 59 cases of coil embolization at unruptured and ruptured aneurysms and two cases of stent insertion into the middle cerebral artery. All the cases were successful without any catheter-related complications.
Conclusion
The Navien catheter is a recently developed catheter that has several strengths compared with previously developed catheters. It provides a more stable environment for endovascular treatment. It provides a cavity sufficient for endovascular treatment devices. Additionally, it is sufficiently flexible to approach tortuous vessels.
Endovascular treatment is one of the most important treatments along with open craniotomy for cerebrovascular surgery.3)7)9) For successful treatment, the proper selection of devices is important as well as the operator's experience. In general, a larger guide catheter is needed when management with multiple devices or bigger devices is required, when a vascular structure is tortuous, or when a target is at the distal level.4) One must consider safety, flexibility, and space availability in choosing proper devices. Devices must be atraumatic to adjacent structures to minimize the possibility of arterial dissection, vasospasm, or other complications.10) In addition, they need to be flexible enough to access tortuous vessels. The NavienŌäó Intracranial Support Catheter (formerly the ReFlex Intracranial Catheter; Covidien Vascular Therapies, Mansfield, MA, USA) is a new intracranial catheter that was used for neurointervention in 61 cases. Therefore, the cases in the Presbyterian Medical Center were analyzed to see if the catheter meets the above standards.
We retrospectively collected data from patients who received coil embolization and stent insertion through Navien catheters between July 2015 and March 2016 at the Presbyterian Medical Center.
All procedures used a triaxial system and were conducted through femoral access. Flexor Shuttle sheath 6-Fr, 0.087-inch Inner diameter (ID) (Cook Medical, Bloomington, IN, USA); Navien 6-Fr, 0.072-inch 105-cm ID distal intracranial catheter (Covidien Vascular Therapies); and microcatheter, 0.027-inch ID, were used. For microcatheters, Echelon Micro Catheter, Rebar Reinforced Micro Catheter, and Prowler Micro Catheter were used. For stents, Solitaire stents were used. Additionally, for guide wires, Silver Speed Hydrophilic Guide Wire and Synchro 2 Guide Wire were used.
We evaluated the aneurysm characteristics, such as ruptured or unruptured state, sizes, and locations. The locations of the guiding catheters, tortuosity of parent vessels, which is defined as a 90-degree turn, hairpin turn, or corkscrew loop, and guide catheter-related complications, including vasospasm or dissection, were evaluated as well.8)
Endovascular treatments were performed using a Navien catheter in 61 cases for 56 patients from July 2015 to March 2016. The mean age was 63.5, and ages ranged from 43 to 82. A total of 15/56 cases (26.8%) involved males, and 41/56 cases (73.2%) involved females. A total of 59/61 (96.7%) cases were aneurysm, and 2/61 (3.3%) cases were stenosis. Among the aneurysm cases, 36/59 (61.0%) cases were anterior circulation and 23/59 (39.0%) cases were posterior circulation. Furthermore, two stenosis cases were found at the proximal middle cerebral arteries (Table 1).
A triaxial support system was used for all 61 cases. Flexor Shuttle sheath 6-Fr, Navien 6Fr 0.072-inch ID catheter, and 0.027-inch ID microcatheter were used. For the microcatheter, an Echelon microcatheter was used for coil embolization. Additionally, Rebar and Prowler microcatheters were used for stent-assisted coil embolization or stent insertion. For guide wires, Silver guide wire for the Echelon microcatheter and Synchro guide wire for the Rebar or Prowler microcatheter were used.
Tortuosity of the common carotid artery (CCA) and internal carotid artery (ICA) was found in 25/61 cases (41.0%) and that of the vertebral artery (VA) was found in 10/61 cases (16.4%). The locations of Navien tips were at the petrous segment of the internal carotid artery (ICA) in 49/61 cases (80.3%), the distal part of the second segment of the VA in 8/61 cases (13.1%), the first segment of the VA in 3/61 cases (0.5%), and failed in 1/61 case (1.6%) (Fig. 1, 2). The VA of the failed case was severely angulated and turned 360 degrees at the subclavian artery, so the catheter was pushed back when initiated (Table 2).
All the cases were successful without any catheter-related complications, such as arterial dissection, vasospasm, and thrombus formation. There were no cases with dissection or thrombus formation. Significant vasospasm after the initiation of the Navien catheters occurred in 2/61 cases (3.3%) not at the VA, but only at the petrous segment of the ICA. They returned to normal status immediately after nimodipine (1 mg/5 mL) injections, and no clinical complications were found (Fig. 3).6)
A Navien 6-Fr 0.072-inch catheter was used for the endovascular treatments in 61 cases. The catheters were located at the petrous segment of the ICA for anterior circulation and at the VA for posterior circulation. A total of 49/61 cases (80.3%) involved the petrous segment of the ICA, 8/61 cases (13.1%) involved the distal part of the second segment of the VA, and 3/61 cases (5.0%) involved the first segment of the VA. The tip of the Navien catheter could not reach the target in 1/61 case (1.6%).
However, complications including thrombus formation or dissection were not found. Significant vasospasm occurred in 2/61 cases (3.3%) at the petrous ICA, but they disappeared after nimodipine injections without causing any complications.6)
Severe vessel tortuosity was found in 35/61 cases (57.4%). Before using Navien catheters, a biaxial system using a guide catheter and microcatheter was used for endovascular treatment. Due to the possibility of dissection, the guide catheter could reach only up to the cervical ICA or subclavian artery, causing catheters to not be maintained or falling, especially in patients with severe vessel tortuosity. Therefore, a more invasive procedure, such as direct carotid puncture, was considered for patients with severe vessel tortuosity.1)2) Therefore, we have recently used a triaxial system instead of a biaxial system.
Safety, flexibility, and space availability should be evaluated for recently developed guide catheters. Devices must be atraumatic to adjacent structures to minimize the possibility of dissection, vasospasm, or other complications. In addition, they need to be flexible enough to access tortuous vessels. A 0.027-inch ID space must be spared for flushing and injection.8)
Other guide catheters include DAC (Stryker Neurovascular/Concentric Medical, Mountain View, CA, USA) and Neuron (Penumbra, Habor Bay Pkwy, Alameda, CA, USA). Compared with other models, Navien catheters have the smallest outer diameter (OD) and biggest ID.4)5) Because of their small OD, Navien catheters can have better function with flushing out from the catheters in a triaxial system and with contrast injections and make atraumatic positioning possible.
Moreover, the relatively big ID enables a bigger microcatheter to be used and leads to better outcomes from roadmap procedures, flushing, and contrast injections.8) Furthermore, the 6-Fr Navien catheter makes stent-assisted or dual-microcatheter coil embolization possible.
The Navien catheter maintained a round shape without changing to an oval shape during the procedure. This characteristic maintains patent lumen in tortuosity for smooth microcatheter manipulation and supports closeness to the treatment site for more stability during device delivery and deployment.4)
Previously developed catheters have weak points. They gain stability from their rigidity, so their stability decreases at curved areas of the CCA, ICA, or VA and vessel trauma or dissection might occur due to these curved areas.4) However, the Navien catheter shows self-anchoring at curved vessels. There were no cases of dissection when the Navien catheter was moved back and forth during coil embolization.
The Navien catheter showed strengths and successful results in endovascular treatment. Nevertheless, it had limitations. Proximal support is required. The procedure can be more complicated, and preparing devices may become more expensive, as a support device, such as shuttle guiding sheath, needs to be used.
The Navien catheter is a recently developed catheter that has several strengths compared with previously developed catheters and may play very important roles in the endovascular treatment of cerebrovascular diseases. It provides a cavity sufficient for endovascular treatment devices. Additionally, it is enough flexible to approach tortuous vessels.
References
1. Blanc R, Piotin M, Mounayer C, Spelle L, Moret J. Direct cervical arterial access for intracranial endovascular treatment. Neuroradiology. 2006 12;48(12):925-929;



2. Cai Y, Spelle L, Wang H, Piotin M, Mounayer C, Vanzin JR, et al. Endovascular treatment of intracranial aneurysm in the elderly: Single-center experience in 63 consecutive patients. Neurosurgery. 2005 12;57(6):1096-1102; discussion 1096-102.



3. Fraser JF, Riina H, Mitra N, Gobin YP, Simon AS, Stieg PE. Treatment of ruptured intracranial aneurysms: looking to the past to register the future. Neurosurgery. 2006 12;59(6):1157-1166; Discussion 1166-7.



4. Colby GP, Lin LM, Huang J, Tamargo RJ, Coon AL. Utilization of the Navien distal intracranial catheter in 78 cases of anterior circulation aneurysm treatment with the Pipeline embolization device. J Neurointerv Surg. 2013 11;5(Suppl 3):iii16-iii21;


5. Hu YC, Stiefel MF. Force and aspiration analysis of the ADAPT technique in acute ischemic stroke treatment. J Neurointerv Surg. 2016 3;8(3):244-246;


6. Ishihara H, Ishihara S, Niimi J, Neki H, Kakehi Y, Uemiya N, et al. Risk factors and prevention of guiding catheter-induced vasospasm in neuroendovascular treatment. Neurol Med Chir (Tokyo). 2015 55(3):261-265;



7. Dinh J, Castenada M, Shimada LM, Torres SE, Strauss BM, Valko JJ, et al. Distal access balloon guide catheter (2015) US Patent No. 8,926,560. Washington, DC: US Patint and Trademark Office.
8. Lin LM, Colby GP, Huang J, Tamargo RJ, Coon AL. Ultra-distal large-bore intracranial access using the hyperflexible Navien distal intracranial catheter for the treatment of cerebrovascular pathologies: a technical note. J Neurointerv Surg. 2014 5;6(4):301-307;


Fig.┬Ā1
Navien support during coil embolization of an unruptured aneurysm on the right internal carotid artery (ICA) bifurcation site in a 76-year-old female. (A) Right common carotid artery (CCA) transfemoral cerebral angiogram (TFCA) showing significant tortuosity of the proximal part. (B) Pre-embolization TFCA showing 3.5 ├Ś 3.0-mm-sized aneurysm on the right ICA bifurcation site. Navien catheter was placed on the petrous segment of right ICA. (C) Post-embolization TFCA showing a totally occluded aneurysmal sac.
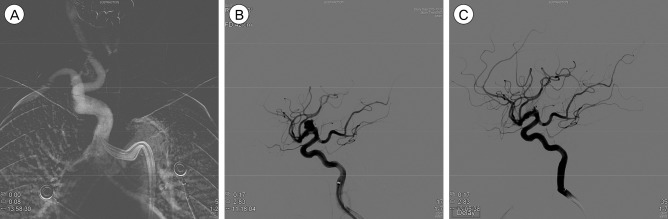
Fig.┬Ā2
Navien support during stent-assisted coil embolization of an unruptured aneurysm on basilar top in a 70-year-old female. (A) Left vertebral artery (VA) transfemoral cerebral angiogram (TFCA) showing significant tortuosity of the proximal part. (B) Pre-embolization TFCA showing 8.2 ├Ś 7.6 mm-sized aneurysm on the basilar top. The aneurysmal sac originated from both posterior cerebral artery (PCA) and superior cerebellar artery (SCA). Navien catheter was placed on the third segment of VA. (C) Post-embolization TFCA showing partially occluded aneurysmal sac. Both PCA and SCA flow were maintained.

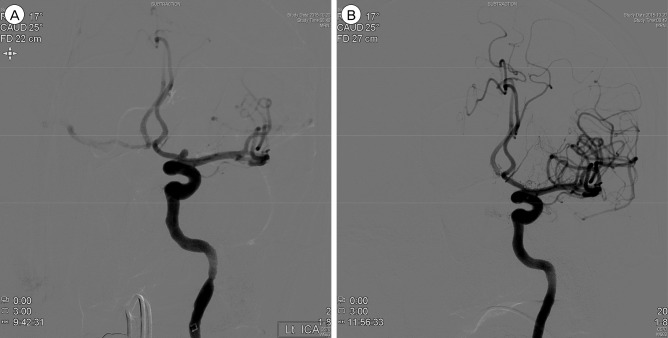
Fig.┬Ā3
Navien support during stent-assisted coil embolization of an unruptured aneurysm on the left proximal anterior cerebral artery in a 79-year-old female. (A) A TFCA showing significant vasospasm post-Navien positioning in the petrous ICA. (B) It returned to normal status immediately after nimodipine (1 mg/5 mL) injection without any post-operative clinical complications. TFCA = transfemoral cerebral angiogram, ICA = internal carotid artery.
Table┬Ā1
Patient demographics and aneurysmal locations
Table┬Ā2
Vessel tortuosity and Navien catheter-tip position
- TOOLS
-
METRICS

-
- 7 Crossref
- 0 Scopus
- 2,498 View
- 27 Download
- Related articles
-
Clinical Analysis of Giant Intracranial Aneurysms with Endovascular Embolization2012 March;14(1)




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



