Rupture of Very Small Intracranial Aneurysms: Incidence and Clinical Characteristics
Article information
Abstract
Objective
Unruptured intracranial aneurysms are now being detected with increasing frequency in clinical practice. Results of the largest studies, including those of the International Study of Unruptured Intracranial Aneurysms, indicate that surgical and endovascular treatments are rarely justified in small aneurysms. However, we have encountered several cases of rupture of small and very small aneurysms in our clinical practice. This retrospective study analyzed the incidence and clinical characteristics of very small ruptured aneurysms.
Materials and Methods
A total of 200 patients with aneurysmal subarachnoid hemorrhage between January 2012 and December 2014 were reviewed. Various factors were analyzed, including the aneurysm location and size as well as the associated risk factors.
Results
The mean age of patients was 56.31 ± 13.78 (range, 25-89) years, and the male to female ratio was 1:2.1. There were 94 (47%) small-sized (< 5 mm), 91 (45.5%) medium-sized (5-9.9 mm), and 15 large-sized (> 10 mm) aneurysms. Of these, 30 (15%) aneurysms were very small-sized (< 3 mm). The most frequent site of aneurysms was the anterior communicating artery (ACoA). However, the proportion of aneurysms at the ACoA was significantly high in very small aneurysms (53.3%, p = 0.013). Hypertension was a significant risk factor for rupture of very small aneurysms (p < 0.001).
Conclusion
About half of our cases of ruptured aneurysms involved the rupture of small and very small aneurysms. The most common site of rupture of very small aneurysm was the ACoA. Rupture of small and very small aneurysms is unpredictable, and treatment may be considered in selected high-risk patients according to factors such as young age, ACoA location, and hypertension.
INTRODUCTION
Unruptured intracranial aneurysms (UIA) are now being detected with increasing frequency in clinical practice. The authors have suggested the following as reasons for this improved detection. As the use of computed tomography (CT) and magnetic resonance imaging (MRI) has become more common, it is now easier to assess the patients' vascular status. In addition, many patients who have risk factors for stroke prefer to undergo vascular status testing to prevent a future stroke. In this clinical setting, neurosurgeons often have to make decisions regarding optimal management, which remains controversial.
The International Study of Unruptured Intracranial Aneurysms (ISUIA) prospectively investigated the natural history of untreated UIA.1) Surprisingly, the risk of rupture of anterior circulation aneurysms < 7 mm in size was 0% in patients with no history of subarachnoid hemorrhage (SAH);20) this result, however, has been criticized.
Results of the largest studies, including those of the ISUIA, indicate that surgical and endovascular treatments are rarely justified in small aneurysms.20) However, we have encountered several cases of rupture of small (< 5 mm) and very small aneurysms (< 3 mm). The aim of this retrospective study was to analyze the incidence and clinical characteristics of very small ruptured aneurysms.
MATERIALS AND METHODS
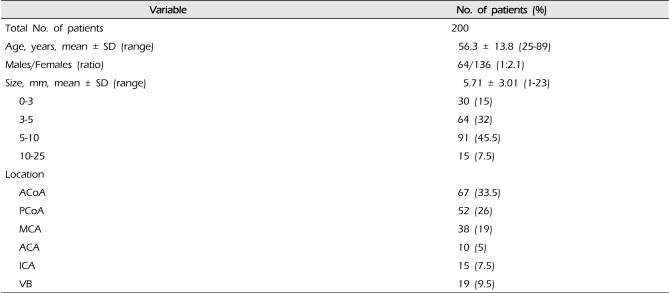
A total of 200 patients with aneurysmal SAH were enrolled in this study between January 2012 and December 2014. Patient information and clinical characteristics are summarized in Table 1. All patients underwent 3-dimensional CT angiography (256 Channels SOMATOM Definition Flash, Siemens, Muenchen, Germany). Based on medical records and CT angiography findings, various factors were analyzed, including the aneurysm location and size as well as the associated risk factors. The aneurysms were classified according to the following categories, as described previously7): small (S; 0-4.9 mm), medium (M; 5-9.9 mm), large (L; ≥ 10 mm), and giant (G; ≥ 25 mm). The small group was further subclassified according to the very small (VS: 0-3 mm) category. The locations of the aneurysms were classified as follows: anterior communicating artery (ACoA), posterior communicating artery (PCoA), all of internal carotid artery (ICA) except PCoA, middle cerebral artery (MCA), anterior cerebral artery (ACA), vertebrobasilar system (VB), including the basilar tip (BT), superior cerebellar artery (SCA), and posterior inferior cerebellar artery (PICA).
All statistical analyses were performed using the SPSS program (version 19.0; SPSS Inc., Chicago, IL, USA). The results are presented as mean ± SD or the number of patients (%). Pearson's chi-square test was used for comparison of categorical variables. Continuous variables were compared among groups using the Student t test and one-way ANOVA. Student t test was used for the intergroup comparison of age. One-way ANOVA was used for analysis of size and location of the aneurysm. Post-hoc comparisons were performed using Bonferroni correction of the significance level. The minimum level of statistical significance was set at p < 0.05.
RESULTS
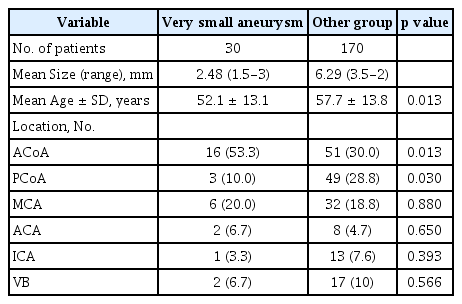
The mean age of patients was 56.31 ± 13.78 years (range, 25-89 years), and the mean ages in the VS and Other groups were 52.1 ± 13.1 years (range, 25-76) and 57.7 ± 13.8 years (range, 27-82), respectively. A statistically significant difference in patient ages was observed between the VS and Other groups. Patients in the very small group were younger than all other patients (p = 0.013). There were 64 men and 136 women. The male to female ratio was 1:2.1, and there was no statistically significant difference in the patient sex between the 2 groups.
Locations of aneurysms
Data on the aneurysms are shown in Table 2. The locations of the aneurysms differed significantly among the groups. The most frequent site of all size aneurysms was ACoA (33.5%), followed by PCoA (26%) and MCA (19%). The most frequent site of small and very small aneurysms was also ACoA. However, significantly high incidence was observed for very small aneurysms (53.3%, p = 0.013). In contrast to aneurysms of all sizes, those of the PCoA were significantly lower among small and very small aneurysms (p = 0.038 and p = 0.030, respectively).
Size distribution of the aneurysms
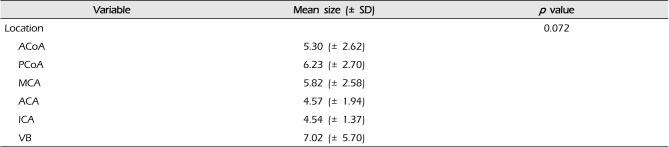
Ninety-four (47%) aneurysms were included in the S category. There were 91 (45.5%) and 15 (7.5%) aneurysms in the M and L categories, respectively. Of the total aneurysms, 30 (15%) were of a very small size. The mean size of all aneurysms was 5.71 ± 3.01 mm (range, 1-23 mm). The mean sizes of small and very small aneurysms were 3.58 ± 0.89 mm and 2.48 ± 0.54 mm, respectively. The mean size of aneurysms larger than 5 mm was 7.60 ± 2.98 mm. No statistical significance was observed between location and size of aneurysms (Table 3).
Risk factors for rupture of aneurysms
Several risk factors including hypertension, previous SAH, multiplicity, and cigarette smoking were evaluated. Table 4 shows various potential risk factors for rupture of aneurysms. In this study, hypertension was a significant risk factor for rupture of very small aneurysms (p < 0.001).
DISCUSSION
Preventive treatment of UIAs with high risk of rupture has become common practice, thus the recent studies on the natural course of UIAs are underestimated.12) It has been suggested that the true rupture rate of UIAs can never be described.16) The most recently reported average lifelong annual rupture rate of UIA was 1.6% for patients and 1.2% for aneurysms.13) Female sex, current smoking, and aneurysm size of ≥ 7 mm in diameter were risk factors for a lifetime SAH. However, the estimation of rupture risk cannot be based solely on the initial size of a UIA. Although 25% of the ruptured UIAs were small at baseline, approximately 77% of the small UIAs grew to ≥ 7 mm in size by the time of the rupture.13)
The risk of rupture is known to increase with the increasing size of an aneurysm.6)20) However, a large number of patients have SAH as a result of rupture of aneurysms with diameters < 5 mm.2)9)10)11)15)18) In the Japanese population, the average annual risk of rupture associated with small UIAs (< 5 mm) was 0.54% overall, 0.34% for single aneurysms, and 0.95% for multiple aneurysms.18) Morita et al.6) reported that the annual rate of rupture of aneurysms <5 mm in the MCA was 0.23% and in the ACA was 0.9% in a Japanese population. Ishibashi et al.7) reported the rupture rate of UIA according to aneurysm size. The annual rupture rate by size was 0.8% (S; < 5 mm), 1.2% (M; 5-9.9 mm), 7.1% (L; ≥ 10 mm), and 43.1% (G; ≥ 25 mm). Of 529 aneurysms, 19 aneurysms ruptured during the follow-up period, and eight (42.1%) out of 19 aneurysms were from the S group. Six (31.6%) were < 3 mm in size.
They concluded that size, history of SAH, and posterior circulation aneurysms were significant risk factors for rupture of aneurysms. However, the size of the UIA should not be the only factor considered when deciding on the treatment strategy for UIAs.
The ISUIA publication has stirred considerable interest in the size of the intracranial aneurysm (IA).1) In general, IA size is an efficient and widely used measurement parameter for IA rupture risk assessment. However, this parameter may miss smaller aneurysms with a higher rupture risk based on the location or relationship with the parent blood vessel. Several studies have reported on the IA rupture risk related to the aneurysm location or parent vessel.3)4)8)14)19) Carter et al.3) explained that aneurysms arising from smaller vessels tend to be small and unstable because they have thinner walls compared with aneurysms originating from a large artery. Therefore, it is suggested that the rupture risk of UIA is related to the IA location and parent vessel diameter. In addition, Ohashi et al.15) reported that the diameter of the ACoA and distal ACA is smaller than that of the MCA and ICA. Thus, aneurysms located in the anterior circulation may bleed before reaching a large size.
The risk of rupture is particularly high in the anterior regions of the circle of Willis with a large percentage of small ruptured aneurysms occurring in the ACoA.8)14)19) Joo et al.8) noted that the ACoA was a much more common location than other sites for aneurysms smaller than 7 mm in size, and the mean size of ACoA aneurysms was the smallest as compared with those at other sites. Forget et al.4) reported that approximately 94% of ruptured aneurysms of the ACoA were small, and 44% were smaller than 5 mm in size. Our result is therefore similar to that of other previous reports. The ACoA location had a higher proportion of aneurysms ≤ 3 mm in size compared to other locations (p = 0.013).
There remains a discrepancy between the rupture rates of small UIA and small ruptured aneurysms diagnosed in practice. The majority of ruptured aneurysms are small in size.5)14)19) One possible explanation is that aneurysm rupture occurs relatively soon after formation, when the aneurysm wall is weaker and before healing processes take place. After this initial stage, aneurysms may reach a somewhat stable condition. This is ascertained by the observation that the rupture risk of UIA is higher during the first year after diagnosis and decreases thereafter.17)
There are many opinions regarding the risk factors associated with rupture of a UIA.1)5)7)13)18) Female Sex, cigarette smoking, multiplicity, previous SAH, family history, and hypertension are some of the proposed risk factors. Although there were other important risk factors, hypertension was found to be a significant risk factor in the prediction of rupture of very small aneurysms (p < 0.001) in our study.
CONCLUSION
About half of our cases of ruptured aneurysms involved the rupture of small and very small aneurysms. The most common site of ruptured very small aneurysm is the ACoA. Predicting the risk of rupture of IAs continues to be a topic of much debate. Although the aneurysm size is a key factor in the prediction of UIA rupture, other factors should be considered when deciding on the treatment strategy for small and very small UIAs. We should keep in mind that the rupture of small and very small aneurysms is unpredictable, and treatment may be considered in selected patients who are at high risk of rupture due to factors such as young age, ACoA location, and hypertension.
Acknowledgements
This paper was supported by Wonkwang University in 2013.
Notes
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.