Combination Treatment for Rapid Growth of a Saccular Aneurysm on the Internal Carotid Artery Dorsal Wall: Case Report
Article information
Abstract
Aneurysms arising from non-branching sites of the supraclinoid internal carotid artery (ICA) are considered rare, accounting for only 0.9-6.5% of all ICA aneurysms. They are thin-walled, broad-based, can easily rupture during surgery, and are referred to as dorsal, superior, anterior, or ventral wall ICA aneurysms, as well as blister-like aneurysms. Various treatment modalities are available for blister-like aneurysms, but with varying success. Here, we report on two cases of saccular shaped dorsal wall aneurysms. Both patients were transferred to the emergency department with subarachnoid hemorrhage because of an aneurysmal rupture. Computed tomography angiography and transfemoral cerebral angiography (TFCA) showed a dorsal wall aneurysm in the distal ICA. We performed clipping on the wrapping material (Lyodura®, temporal fascia). Follow-up TFCA showed rapid configuration changes of the right distal ICA. Coil embolization was also performed as a booster treatment to prevent aneurysm regrowth. Both patients were discharged without neurologic deficit. No evidence of aneurysm regrowth was observed on follow-up TFCA at two years. Dorsal wall ICA aneurysms can change in size over a short period; therefore, follow-up angiography should be performed within the short-term. In cases of regrowth, coil embolization should be considered as a booster treatment.
INTRODUCTION
Of the internal carotid artery (ICA) aneurysms, those arising from the non-branching sites of the supraclinoid ICA are considered rare, accounting for only 0.9-6.5% of all ICA aneurysms.1)16) These aneurysms are referred to by many names, including dorsal, superior, anterior, or ventral wall ICA aneurysms, as well as blood blister-like aneurysms (BBAs).3)4)8)12)13)16,17),18) There are two morphological types based on angiographic appearance: blood blister and saccular types, which include ordinary berry aneurysms.18)22) Blister type aneurysms are thin-walled, broad-based, and rupture easily during an operation, resulting in high morbidity and mortality,1)18)21) while the saccular type can be safely clipped owing to the firm neck.1)18) However, the natural history of BBAs has not been defined. Angiographic morphological changes can be found on serial cerebral angiography.1)18) Various treatment modalities are available for blister-type aneurysms, however, their outcomes vary.1)2)16)18)19)23) Here, we report on two cases of saccular-shaped dorsal wall aneurysm with rapid morphological changes that were treated by clipping on the wrapping material followed by coil embolization.
CASE REPORTS
Case 1
A 39-year-old woman was admitted for a sudden-onset headache and generalized tonic-clonic seizure. On admission, no focal neurologic deficits were observed, only a drowsy state. The initial brain computed tomography (CT) showed a subarachnoid hemorrhage (SAH) in the basal cistern, suprasellar cistern, and right sylvian fissure. Subsequent CT angiography showed a dorsal wall aneurysm on the right ICA and two dissecting aneurysms on the bilateral distal vertebral arteries. Transfemoral cerebral angiography (TFCA) performed the next day confirmed a broad-based, saccular aneurysm measuring 2.5 mm in size on the dorsal wall of the right ICA and dissecting aneurysms on the bilateral vertebral arteries (Fig. 1A). On day 2 after rupture, we performed a right pterional craniotomy for direct clipping. The aneurysm was completely dissected; however, the clip was not applied because of the very thin wall and neck (Fig. 1B). Finally, she was treated with clipping after wrapping with the temporal fascia. She made a full postoperative recovery. Two weeks later, she underwent stent-assisted coil embolization for the left VA aneurysm. Follow-up TFCA performed one month after onset showed that the right ICA aneurysm had increased in size (Fig. 1C). We performed coil embolization without a stent (Fig. 1D), and she was discharged without any neurological focal signs.
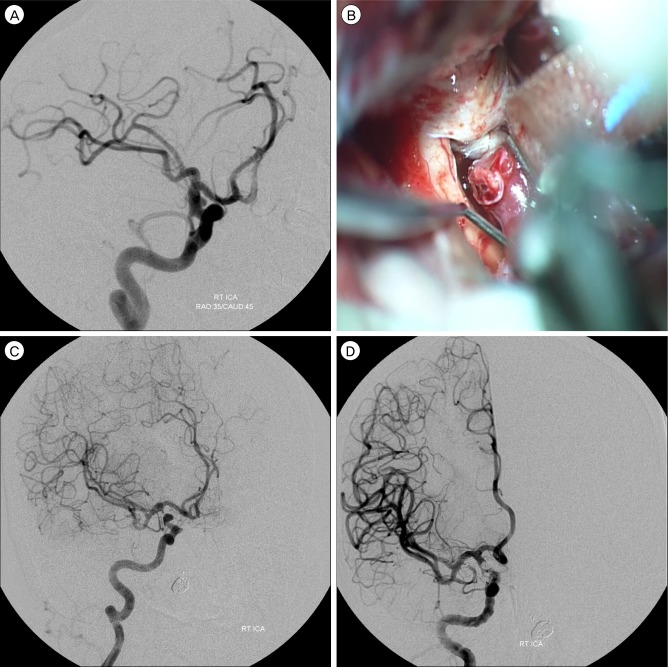
(A) Transfemoral cerebral angiography (TFCA) showing a broad-based aneurysm in the right distal internal carotid artery (ICA). (B) Intraoperative photo showing the dissected aneurysm. (C) Follow-up TFCA showing growth of the right distal ICA aneurysm. (D) Embolization was performed for the right ICA aneurysm.
Case 2
A 58-year-old woman was transferred to our emergency department with sudden onset headache and vomiting. On initial neurological examination, her mental status was drowsy, but no focal neurological deficits were observed. The initial brain CT showed diffuse SAH and intracerebral hemorrhage (ICH) in the right temporal area. Subsequent CT angiography showed subtle bulging at the right ICA. TFCA performed the following day showed the same finding as the previous CT angiography (Fig. 2A). Follow-up angiography for both carotid ICAs, performed two weeks after onset, showed a definite aneurysm measuring 3.9 mm in size at the location of the previous bulging lesion of the right ICA (Fig. 2B). Craniotomy was performed for direct clipping. During the operation, the aneurysm was completely dissected, and its neck was relatively firm. We attempted to perform careful clipping of the aneurysmal neck directly, but a slight tear occurred; therefore, we performed the clipping on the wrapping with Lyodura® (B.Braun, Melsungen, Germany) after the bleeding had ceased (Fig. 2C). She made a full recovery postoperatively. One month later, an increase in aneurysm size was observed on the follow-up angiography (Fig. 2D). She underwent simultaneous coil embolization without a stent (Fig. 2E), and no evidence of aneurysmal regrowth was observed by TFCA during the 2-year follow-up period (Fig. 2F).
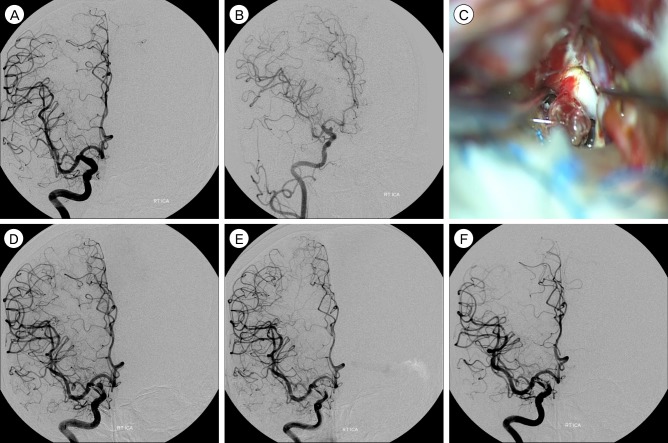
(A) Transfemoral cerebral angiography (TFCA) showing no definite aneurysm, but there is evidence of a subtle bulging lesion in the right internal carotid artery (ICA). (B) Follow-up TFCA showing an aneurysm in the right distal ICA. (C) Intraoperative photo showing the saccular aneurysmal rent. (D) Follow-up angiography at one month showing growth of the aneurysm (E) Coil embolization was performed. (F) Follow-up angiography at two years showing no residual aneurysm.
DISCUSSION
Aneurysms arising from the non-branching site of the supraclinoid ICA account for only 0.5% of ruptured intracranial aneurysms.15) Those that are broad-based and small are called blister aneurysms.2)10) Of the two types of these aneurysms based on angiographic appearance (blister and saccular types), BBAs have a number of unique clinical features, including right side dominancy; higher frequency in women; associations with hypertension, arteriosclerosis, and ICA dissection; highly unstable walls; poorly defined necks; and high morbidity and mortality.1)3)16)18)22)
Although the exact pathogenesis of these aneurysms has not been clearly defined, Ishigawa et al. reported that these lesions are focal wall defects instead of true aneurysms because they might be covered with thin fibrous tissue. The authors also suggested that arterial dissection can cause BBAs. According to some reports, a focal wall defect resulting from a small ulceration and continuous hemodynamic stress may contribute to development of BBAs at the anteromedial, anterolateral, or anterior wall of the supraclinoid ICA.1)6) However, Regelsberger et al. suggested that the arteriosclerotic effect is an important factor in development of blister aneurysms, rather than arterial wall dissection, at this unusual site.20) An aneurysm that initially presents as a blister type can show rapid morphological change to a saccular type along with rapid growth in size;1)7)18) these aneurysms have been regarded as false aneurysms with extremely unstable walls, such as with BBAs.9) While it has been suggested that such a morphological change could be caused by the growth and organization of a blood clot surrounding a focal wall defect,18) it is also possible that a partial occlusion and recanalization may lead to development of an initial bulge in a blister type aneurysm.7) Both of the current cases occurred in the right-sided ICA and appeared as true saccular-shaped aneurysms with extremely unstable walls and necks, which differ from the typical saccular type that has a firm neck. In addition, there was no evidence of ICA dissection, arteriosclerosis, partial occlusion, or thrombosis during surgery, all of which are characteristic of BBAs. We believe that hemodynamic stress of unknown origin at the lesion site, which had a thin wall and neck, could have played a key role in the morphological changes.
Blister-like aneurysms are easily misdiagnosed by MRA and CTA; therefore, TFCA should be performed in SAH patients with negative CTA or MRA findings. Diagnosis of BBAs can be challenging because of their less obvious bulging; the only preoperative indication of a blister-like aneurysm is an unusual appearance at a location other than the arterial branches.20) However, typical angiographic findings related to BBAs include a thin bleb, a bulging appearance with a wide base, an irregular bulge of the anterior wall of the ICA, and rapid morphological changes.13)
Although various treatment modalities to secure BBA have been described, including an encircling clip graft, surgical trapping, direct surgical clipping, endovascular coiling, and extracranial-intracranial (EC-IC) bypass surgery, the unstable wall presents challenges in determining the best approach.1)3)5)7)16)18) Some authors have recommended clipping of the ICA in a parallel fashion to prevent tearing of the aneurysmal neck, however, this can result in a poor outcome because of a premature rupture or parent vessel stenosis.1)16)18) Successful repair of an aneurysmal rupture at its base by direct suture and an encircling clip has been reported, 24) while the direct microsuture technique has also been successful for premature BBA rupture during surgery.23) For a small aneurysm and short, temporary entrapment, direct arterial repair should be performed.4) Wrapping alone is not effective to secure an aneurysm and is significantly associated with postoperative bleeding.18) Direct clipping has been unsuccessful because of extremely unstable walls and necks; therefore, to reinforce BBAs, clipping has been used after wrapping the entire ICA, using muscle, fascia, gauze, cellulose fabric, Gore-Tex, or Lyodura®. However, complications include regrowth, re-rupture, perforator injury, and difficulty in confirming the margin for wrapping.1)18) However, clipping on the wrapping was not effective in the current cases, as evidenced by the continued growth observed on follow-up angiography.
Endovascular coil embolization is another treatment option for dorsal wall ICA aneurysm; however, because of the unstable aneurysmal wall and potential of incomplete packing with a residual neck, the risk of rupture during coiling is very high.9)19)21) The endurance and effectiveness of coil embolization for management of dorsal wall ICA aneurysms remains controversial and dangerous;7)9)21) Management of aneurysm regrowth and re-rupture of a dorsal wall ICA aneurysm by coil embolization has been reported. Good outcomes with reconstructive endovascular treatment using a stent-within-stent technique for BBA have been reported;6) the authors suggested that healing and thrombosis is facilitated by the unstable aneurysm neck and reduction in flow impingement by multiple-stent insertion. Another treatment option for BBAs involves surgical ICA occlusion or endovascular ICA occlusion,18)19) which is considered an appropriate method if the collateral circulation is intact.19) However, the balloon occlusion test to confirm collateral circulation does not always guarantee the best outcome and can cause delayed ischemic complications, including cerebral infarction, despite a good result.11)12) The combination of wrapping and delayed coil embolization is reportedly effective for these aneurysm types.13)14) In two cases treated using clipping on wrapping and delayed coil embolization, there was no procedural rupture, and no regrowth was observed on the 2-year follow-up angiogram. The authors suggested that the initial wrapping material reinforced the weak aneurysmal wall and functioned as a barrier, helping to avoid a procedural rupture during the coil embolization.
CONCLUSION
Dorsal wall ICA aneurysms can change in size over a short time period; therefore, short-term follow-up is recommended. Unlike the saccular type BBAs with a firm neck, saccular-shaped BBAs with a weak neck can rupture easily; therefore, direct clipping can be hazardous. Although clipping on wrapping material is one treatment option, it may not prevent aneurysmal regrowth. In the case of regrowth, coil embolization should be considered as a booster treatment.
