1. Aldape KD, Plate KH, Vortmeyer AO, Zagzag D, Neumann HPH. Hemangioblastoma. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, editors. WHO Classification of tumours of the central nervous system. 4th ed. Lyon: International agency for research on cancer (IARC); 2007. p. 184-186.
3. Campos WK, Linhares MN. Sporadic intramedullary spinal cord hemangioblastoma in a newborn. Pediatr Neurosurg. 2010 11;46(5):385-389;


5. Cornelius JF, Saint-Maurice JP, Bresson D, George B, Houdart E. Hemorrhage after particle embolization of hemangioblastomas: comparison of outcomes in spinal and cerebellar lesions. J Neurosurg. 2007 6;106(6):994-998;


6. Cushing H, Bailey P. Tumors arising from blood vessels in the brain: angiomatous malformations and hemangioblastomas. Springfield, IL: Charles C Thomas; 1928.
8. Drake CG, Peerless SJ. Giant fusiform aneurysms: review of 120 patients treated surgically from 1965 to 1992. J Neurosurg. 1997 8;87(2):141-162;


9. Elhammady MS, Wolfe SQ, Ashour R, Farhat H, Moftakhar R, Lieber BB, et al. Safety and efficacy of vascular tumor embolization using Onyx: is angiographic devascularization sufficient? J Neurosurg. 2010 5;112(5):1039-1045;


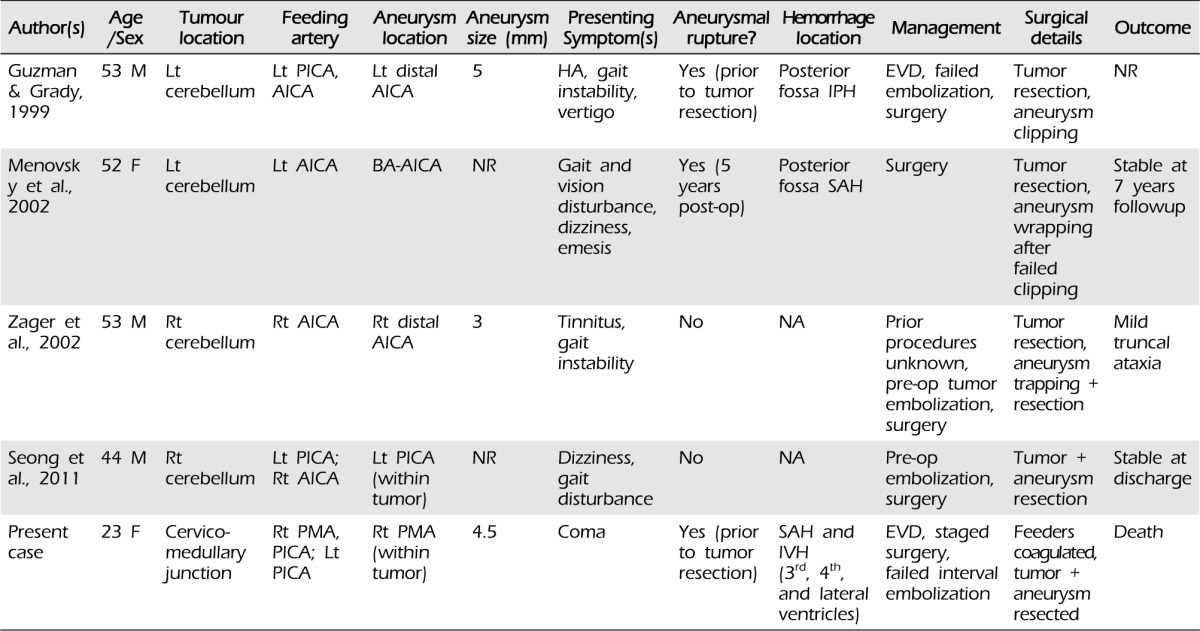
11. Guzman R, Grady MS. An intracranial aneurysm on the feeding artery of a cerebellar hemangioblastoma. Case report. J Neurosurg. 1999 7;91(1):136-138;


12. Menovsky T, André Grotenhuis J, Bartels RH. Aneurysm of the anterior inferior cerebellar artery (AICA) associated with high-flow lesion: report of two cases and review of literature. J Clin Neurosci. 2002 3;9(2):207-211;


13. Montano N, Doglietto F, Pedicelli A, Albanese A, Lauretti L, Pallini R, et al. Embolization of hemangioblastomas. J Neurosurg. 2008 5;108(5):1063-1064;


15. Ogawa T, Fujita H, Inugami A, Shishido F, Higano S, Uemura K. Anomalous origin of the posterior inferior cerebellar artery from the posterior meningeal artery. AJNR Am J Neuroradiol. 1991 Jan-Feb;12(1):186


17. Seong Eom K, Won Kim D, Sung Choi S, Ha Choi K, Young Kim T. Preoperative embolization of a cerebellar hemangioblastoma using Onyx: case report and literature review. Neurol Neurochir Pol. 2011 May-Jun;45(3):292-296;


19. Tsutsumi M, Kazekawa K, Aikawa H, Iko M, Kodama T, Nii K, et al. Development of unusual collateral channel from the posterior meningeal artery after endovascular proximal occlusion of the posterior inferior cerebellar artery. Neurol Med Chir (Tokyo). 2007 11;47(11):503-505;


20. Vates GE, Berger MS. Hemangioblastomas of the central nervous system. In: Winn HR, editors. Youmans Neurological Surgery. 5th ed. Philadelphia: Saunders; 2004. p. 1053-1066.
21. Zager EL, Shaver EG, Hurst RW, Flamm ES. Distal anterior inferior cerebellar artery aneurysms. Report of four cases. J Neurosurg. 2002 9;97(3):692-696;







 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



