 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 16(3); 2014 > Article |
|
Abstract
Objective
The aim of this study was to investigate the correlation between meteorological factors and occurrence of spontaneous intracerebral hemorrhage (ICH) according to age.
Materials and Methods
We retrospectively analyzed the records of 735 ICH patients in a metropolitan hospital-based population. Observed and expected numbers of ICH patients were obtained at 5℃ intervals of ambient temperature and a ratio of observed to expected frequency was then calculated. Changes in ambient temperature from the day before ICH onset day were observed. The Wilcoxon-Mann-Whitney test was used to test differences in meteorological variables between the onset and non-onset days. The Kruskal-Wallis test was used for comparison of meteorological variables across gender and age.
Results
ICH was observed more frequently (observed/expected ratio ≥ 1) at lower mean, minimum, and maximum ambient temperature (p = 0.0002, 0.0003, and 0.0002, respectively). Significantly lower mean, minimum, and maximum ambient temperature, dew point temperature, wind speed, and atmospheric pressure (p = 0.0003, 0.0005, 0.0001, 0.0013, 0.0431, and 0.0453, respectively) was observed for days on which spontaneous ICH occurred. In the subgroup analysis, the ICH onset day showed significantly lower mean, minimum, and maximum ambient temperature, dew point temperature, relative humidity, and higher atmospheric pressure in the older (≥ 65 years) female group (p = 0.0093, 0.0077, 0.0165, 0.0028, 0.0055, and 0.0205, respectively).
Spontaneous intracerebral hemorrhage (ICH) is a major cause of mortality and disability in neurosurgical practice. The relationship of meteorological factors and spontaneous ICH has been studied extensively. However, the results varied according to climate, geography, and study design. Seasonal variation has been found in many countries.2)6)10)15)19)20) Various meteorological factors, including ambient temperature, atmospheric pressure, and change of diurnal temperature were also demonstrated to show association with the incidence of spontaneous ICH.4)6)7)11)12) In contrast, a single study failed to show a relationship between meteorological variables and the occurrence of ICH.3)
In addition, age is a demographic risk factor in the occurrence of ICH.5) As in most developed countries, the general population of South Korea is aging. Therefore, interest in public health is likely to increase in the older age group. It is worthwhile to have knowledge of how the occurrence of ICH is influenced by meteorological factors in the older age group, because it might be helpful in promoting public health in a metropolitan city.
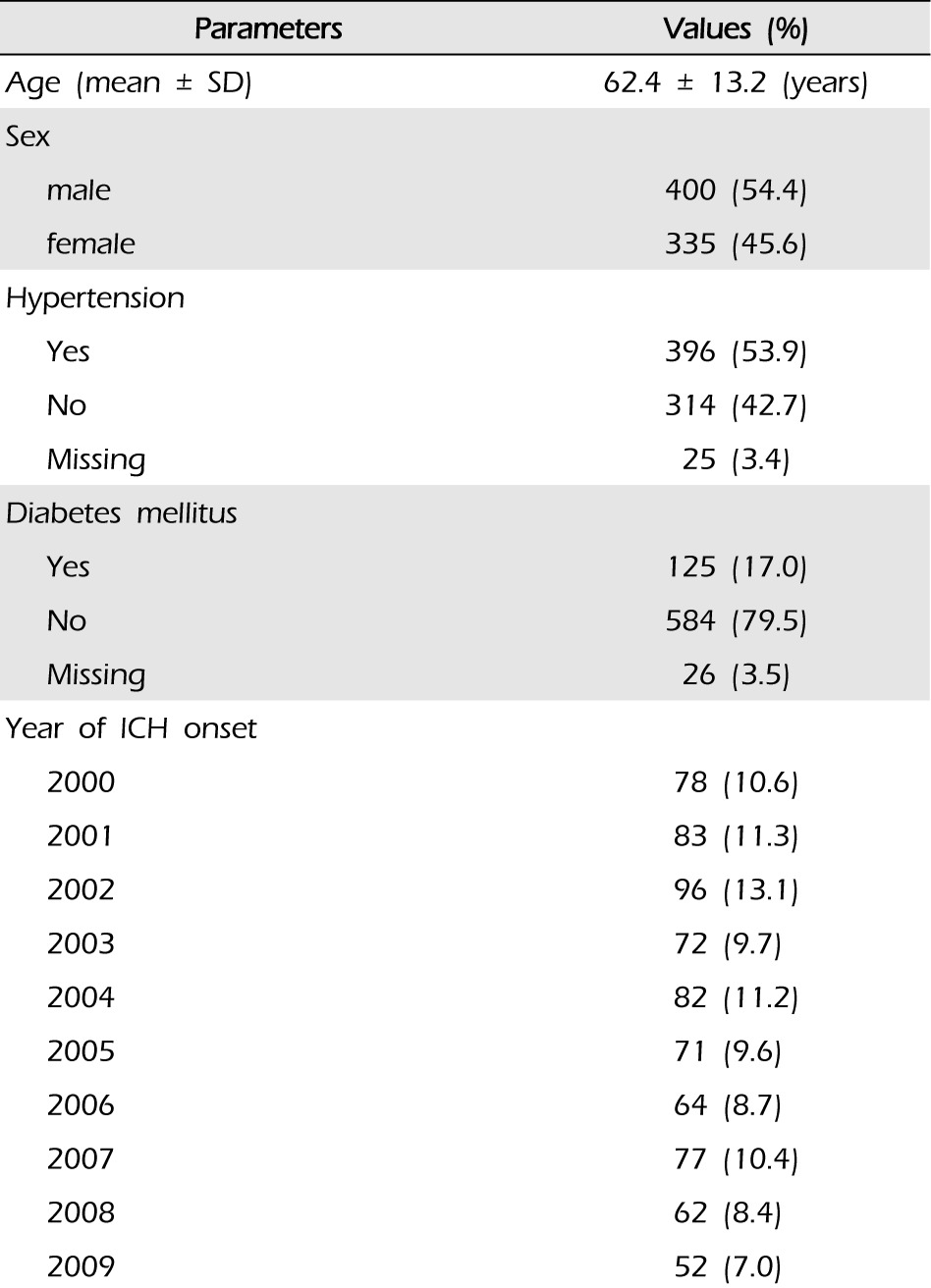
The study population comprised 735 patients admitted to our institution suffering from spontaneous ICH from January 2000 to December 2009. All patients were evaluated by neurosurgeons and underwent workup by brain computed tomographic (CT) scans or magnetic resonance imaging. We excluded secondary causes of ICH (due to cerebral aneurysm, arteriovenous malformation, moyamoya disease, and trauma) based on CT findings and past medical history. When necessary, cerebral angiography was performed to exclude other etiologies. We also excluded patients for whom the onset day was not known and patients who were transferred in from outside the city. We retrospectively analyzed the clinical data of these patients, including age, sex, past history of hypertension, diabetes mellitus, and the date of ICH onset.
Data on ambient temperature (℃), dew point temperature (℃), daily precipitation amount (mm), wind speed (m/s), relative humidity (%), and atmospheric pressure (hPa) from 1 January 2000 to 31 December 2009 in Seoul, where the hospital was located, were obtained from the Korea Meteorological Administration. The hospital is located in northeast Seoul. The distance between the Seoul meteorological observatory and the hospital is approximately 12 km. For statistical analysis, we used meteorological data measured at the Seoul meteorological observatory.
Changes in mean, minimum, and maximum temperatures were calculated as the differences between the date of and the day before the onset of ICH, i.e., mean temperature change was calculated as mean temperature of onset day - mean temperature of the day before onset.
Observed and expected numbers of ICH patients were obtained by 5℃ intervals of ambient temperature and changes in mean, minimum, and maximum temperature. Subsequently, the ratio of observed to expected frequencies was calculated. Expected frequency was calculated as Eij=(Ri × Cj) / T; where Eij is the expected frequency of the cell in the ith row and the jth column, Ri is the total number of subjects in the ith row, Cj is the total number of subjects in the jth column, and T is the total numbers of the whole table.
Non-parametric significance tests were used for comparison of meteorological differences between groups, since the meteorological factors were not normally distributed. The chi-square test was used for evaluation of observed versus expected numbers of ICH events by ambient temperature. The Wilcoxon-Mann-Whitney test was used to test differences in meteorological variables between the onset and non-onset days. The Kruskal-Wallis test was used for comparison of meteorological variables between age groups by gender. Analyses were performed using SAS statistical software (SAS Institute Inc., Cary, NC, United States). A probability value less than 0.05 was considered statistically significant.
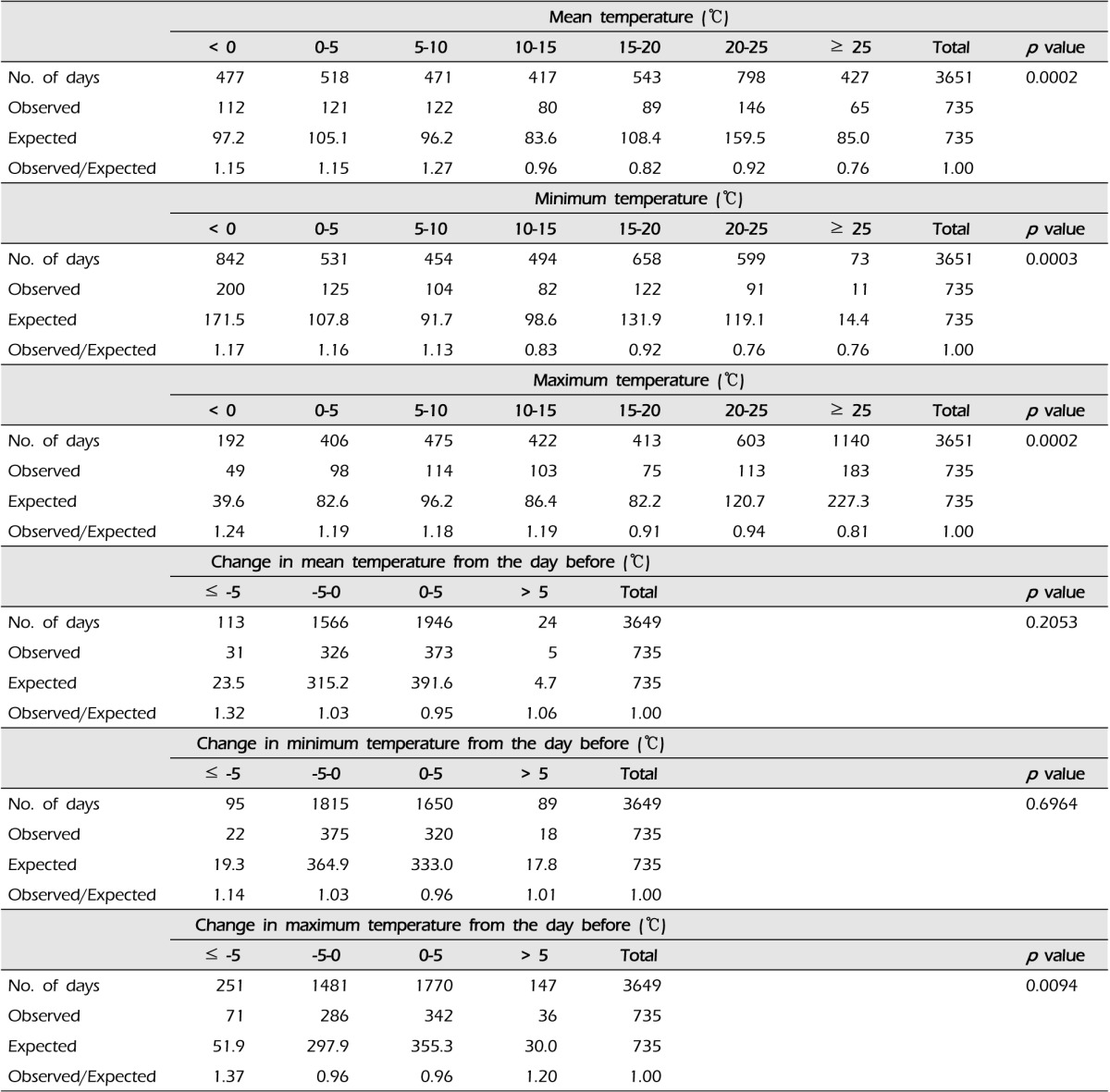
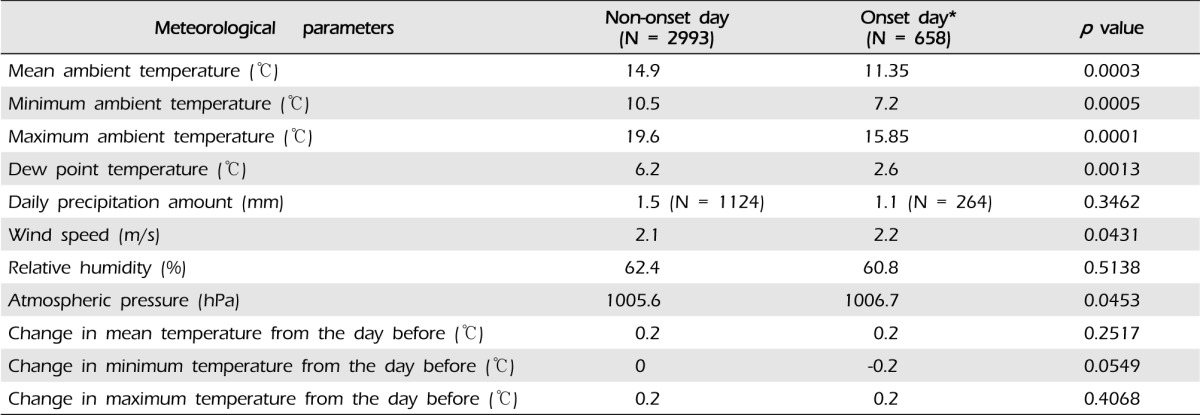
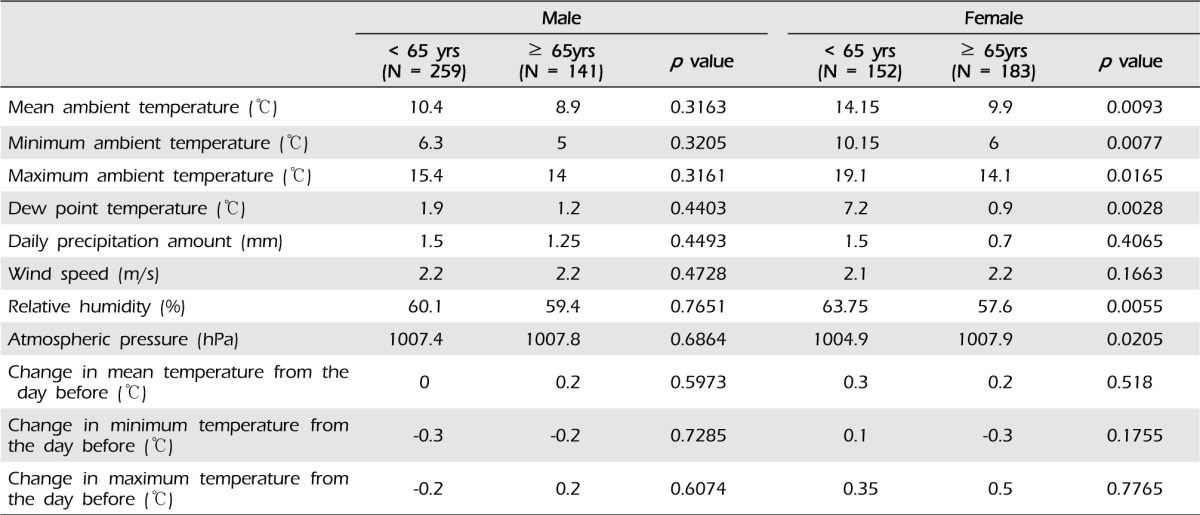
We analyzed 735 patients (400 men, 335 women) with a mean age of 62 ± 13 years. Clinical data of 735 enrolled patients are shown in Table 1. ICH was observed more frequently (observed/expected ratio ≥ 1) at lower mean, minimum, and maximum ambient temperature (p = 0.0002, 0.0003, and 0.0002, respectively). When the change in maximum temperature from the day before was ≤ -5 or ≥ 5℃, ICH was observed more frequently (p = 0.0094) (Table 2). Significantly lower mean, minimum, and maximum ambient temperature, lower dew point temperature, higher wind speed, and higher atmospheric pressure (p = 0.0003, 0.0005, 0.0001, 0.0013, 0.0431, and 0.0453, respectively) were observed on days on which spontaneous ICH occurred (Table 3). In the subgroup analysis, the ICH onset day showed significant differences in mean, minimum, and maximum ambient temperature, dew point temperature, relative humidity, and atmospheric pressure in the older (≥ 65 years) female group compared with other groups (p = 0.0093, 0.0077, 0.0165, 0.0028, 0.0055, and 0.0205, respectively) (Table 4).
In this study, we found a significant association between lower ambient temperatures and the occurrence of ICH in a metropolitan city in South Korea. Other meteorological parameters, including dew point temperature, wind speeds, and atmospheric pressure also showed significant association with the occurrence of ICH.
The relevant literature provides inconsistent results for the relationship between ICH and ambient temperature. In a retrospective study, ICH tended to occur more frequently than expected at lower ambient temperatures.14) A multi-community cohort study conducted in Japan reported an association of low ambient temperature and high annual rainfall with increased risk of stroke incidence in women.10) A study conducted in Hong Kong showed a strong, negative linear association of daily temperature with hemorrhagic stroke admission.4) A population-based study conducted in northern Portugal found that the incidence of ICH increased by 11.8% for each degree drop in the ambient temperature on the preceding day.9) This association is generally explained by the fact that low ambient temperature induces elevation of blood pressure by the constriction of peripheral vessel and changes in blood viscosity, platelet count, and catecholamine secretion.1)8) In contrast, Field et al.3) reported that ICH occurrence did not show any association with changes in weather parameters. They concluded that these discrepancies might be explained by confounding factors such as socioeconomic conditions, emotional stress, genetic factors, and study design.
Our study also found an increase in ICH with higher atmospheric pressure. Consistent with our findings, a study from Spain showed that the incidence of ICH was related to the daily increases in atmospheric pressure.7) Nakaguchi et al.12) showed that the incidence of ICH tends to be high when atmospheric pressure is above the yearly mean value for two-three days preceding the day of onset, or that the pressure is high on the day of onset. They interpreted this finding by suggesting that peripheral vessels are compressed and constricted under high atmospheric pressure causing high blood pressure and increased sympathetic tone. In addition, oxygen saturation can increase when engaging in excessive physical activity. Therefore, high atmospheric pressure is considered to increase the incidence of ICH by these direct and indirect effects. In 2012, Goggins et al.4) found an increase in hemorrhagic stroke admissions with increased air pressure from the day before stroke onset. They emphasized the possibility that changes in atmospheric pressure could cause changes in pressure across the vessel wall and in endothelial function, leading to rupture.4)7)
One of the interesting results of our study is that ICH tends to occur more frequently on days with faster wind speed. In Seoul, the wind speed is usually faster during the spring and winter than during other seasons.13) Therefore, low ambient temperature with faster wind speed may increase the occurrence of ICH in this moderate climate area.
In addition, we found that the older female group is more susceptible to ICH in lower ambient temperature, compared with other groups. Some investigators reported that seasonal and temperature variations were more noticeable in older patients.4)16)20) There is no clear explanation for this finding; however, Passero et al.16) suggested that the elderly might have exaggerated physiological responses to cold weather, with greater increases in blood pressure, as shown in studies of myocardial infarction and ischemic stroke.15)18) A hospital-based study found that the incidence of ICH was prominent in the older population, and hypothesized the possibility that older age is more susceptible to environmental changes.19) A recent cohort study conducted in Japan reported that females were more susceptible to lower ambient temperature in stroke incidences than males independent of conventional risk factors.10) There is no clear explanation for this finding, however, this appears to be caused by the difference of cold-induced vascular reaction according to gender.17)
Our study has certain limitations, apart from the inherent limitations of the retrospective design. First, this hospital-based study may have underestimated the true incidence of ICH in the community. Second, the meteorological factors measured in one area could not represent the ambient temperature actually experienced by the ICH patient. Third, it would be difficult to know the exact time of ICH onset and the setting in which the hemorrhagic event began (i.e. indoor or outdoor, cold protection devices, and emotional stress). Fourth, socioeconomic factor of the patients may contribute to the occurrence of ICH in a metropolitan city. In this study, we did not investigate this factor. These limitations may have confounded the study results.
The occurrence of spontaneous ICH is closely associated with meteorological factors, and the older females are more susceptible to lower ambient temperature. Further studies with multi-center data may be helpful in elucidating the risk of the occurrence of ICH and promote public health in a community.
References
1. Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J (Clin Res Ed). 1982 10;285(6346):919-923.



2. Fang CW, Ma MC, Lin HJ, Chen CH. Ambient temperature and spontaneous intracerebral haemorrhage: a cross-sectional analysis in Tainan, Taiwan. BMJ Open. 2012 6;2(3):e000842.



4. Goggins WB, Woo J, Ho S, Chan EY, Chau PH. Weather, season, and daily stroke admissions in Hong Kong. Int J Biometeorol. 2012 9;56(5):865-872;



5. Hanggi D, Steiger HJ. Spontaneous intracerebral haemorrhage in adults: a literature overview. Acta Neurochir (Wien). 2008 4;150(4):371-379; discussion 379.



6. Im SB, Yun IG, Lee KS, Bae HG, Byun BJ. [Relationship between spontaneous cerebral hemorrhage and climatic factor]. J Korean Neurosurg Soc. 1996 9;25(9):1786-1793; Korean.
7. Jimenez-Conde J, Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Subirana I, et al. Weather as a trigger of stroke. Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis. 2008 26(4):348-354;


8. Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Murphy M, Chelliah R. Increased in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombolysis in winter. Br Med J (Clin Res Ed). 1984 11;289(6456):1405-1408.



9. Magalhaes R, Silva MC, Correia M, Bailey T. Are stroke occurrence and outcome related to weather parameters? Results from a population-based study in northern portugal. Cerebrovasc Dis. 2011 32(6):542-551;


10. Matsumoto M, Ishikawa S, Kajii E. Cumulative effects of weather on stroke incidence: a multi-community cohort study in Japan. J Epidemiol. 2010 20(2):136-142;



11. Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S. Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke. 2011 3;42(3):593-600;


12. Nakaguchi H, Matsuno A, Teraoka A. Prediction of the incidence of spontaneous intracerebral hemorrhage from meteorological data. Int J Biometeorol. 2008 3;52(4):323-329;



13. Oh HS, Chim YS, Kim JY, Chang YS. Determination of upward and downwind areas of Seoul, Korea using trajectory analysis. Asian J Atmos Environ. 2010 9;4(2):89-96.


14. Ohwaki K, Yano E, Murakami H, Nagashima H, Nakagomi T. Meteorological factors and the onset of hypertensive intracerebral hemorrhage. Int J Biometeorol. 2004 11;49(2):86-90;



15. Pan WH, Li LA, Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. 1995 2;345(8946):353-355;


16. Passero S, Reale F, Ciacci G, Zei E. Differing temporal patterns of onset in subgroups of patients with intracerebral hemorrhage. Stroke. 2000 7;31(7):1538-1544;


17. Sato F, Matsushita S, Hyodo K, Akishima S, Imazuru T, Tokunaga C, et al. Sex difference in peripheral arterial response to cold exposure. Circ J. 2008 8;72(8):1367-1372;


18. Sheth T, Nair C, Muller J, Yusuf S. Increased winter mortality from acute myocardial infarction and stroke: the effect of age. J Am Coll Cardiol. 1999 6;33(7):1916-1919;


- TOOLS
-
METRICS

-
- 9 Crossref
- 0 Scopus
- 65,535 View
- 23 Download
- Related articles
-
Management Strategy of Spontaneous Subcortical Intracerebral Hemorrhage.2002 September;4(2)
Pathophysiology of Spontaneous Intracerebral Hemorrhage.2006 March;8(1)
Diurnal and Seasonal Variations in the Onset of Spontaneous Intracerebral Hemorrhage.2007 March;9(1)
Clinical Analysis of Spontaneous Intracerebral Hemorrhage in Young People.2008 September;10(3)




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



