 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 23(2); 2021 > Article |
|
Abstract
Giant internal carotid artery (ICA) aneurysms are complex vascular lesions which are difficult to treat with open as well as endovascular surgery. Parent vessel occlusion is a well-established treatment option for such aneurysms. However, there have been a few reported cases of ruptured aneurysms related to the persistent retrograde filling after parent vessel occlusion. We report a case which highlights the usage of the flow diverter stent as a potential treatment strategy for the management of retrograde filling of aneurysms. A 54-year-old female was found to have a giant left ICA aneurysm on a brain magnetic resonance imaging during workup for headaches. She underwent occlusion of the left ICA proximal to the aneurysm using multiple coils. However, follow up angiograms after 6 months and 2 years demonstrated persistent retrograde filling of the left ICA aneurysm through the posterior communicating (PCOM) artery. Eventually, she was successfully treated with a flow diverter stent across the PCOM artery into the distal ICA. Follow up angiogram after 6 months showed patent flow in the PCOM artery and the distal ICA. with complete occlusion of the aneurysm. Using a flow diverter stent after insufficient parent vessel occlusion for giant intracranial aneurysms may be a feasible treatment option and an addition to the neurovascular treatment armamentarium.
Giant internal carotid artery (ICA) aneurysms are rare. Management of these aneurysms poses significant challenges for open as well as endovascular treatment. Traditionally, before the advent of flow diverter stents, proximal parent vessel occlusion (PPVO) was one of the main treatment options of these complex aneurysms [4,8]. With the advancement of flow diverter stents technology, endovascular management of these aneurysms has revolutionized significantly. Although most of these aneurysms can now be treated with flow diverter stents [1,3], PPVO is still a valid option, particularly for aneurysms with complex anatomy or when the cost of treatment is factored in the choice of treatment. One of the main concerns for PPVO treatment is the risk of retrograde filling of the ICA aneurysm through collateral channels. These retrograde filling aneurysms are challenging to treat and mostly managed conservatively with serial follow up angiograms. We hereby report a case of giant ICA aneurysm, which was initially treated with PPVO but continued to fill retrogradely through a patent posterior communicating (PCOM) artery. This was eventually successfully treated with a flow diverter stent across the PCOM artery into the distal ICA. There is no previous description of such treatment method in the literature for management of retrograde filling of giant ICA aneurysms following parent vessel occlusion.
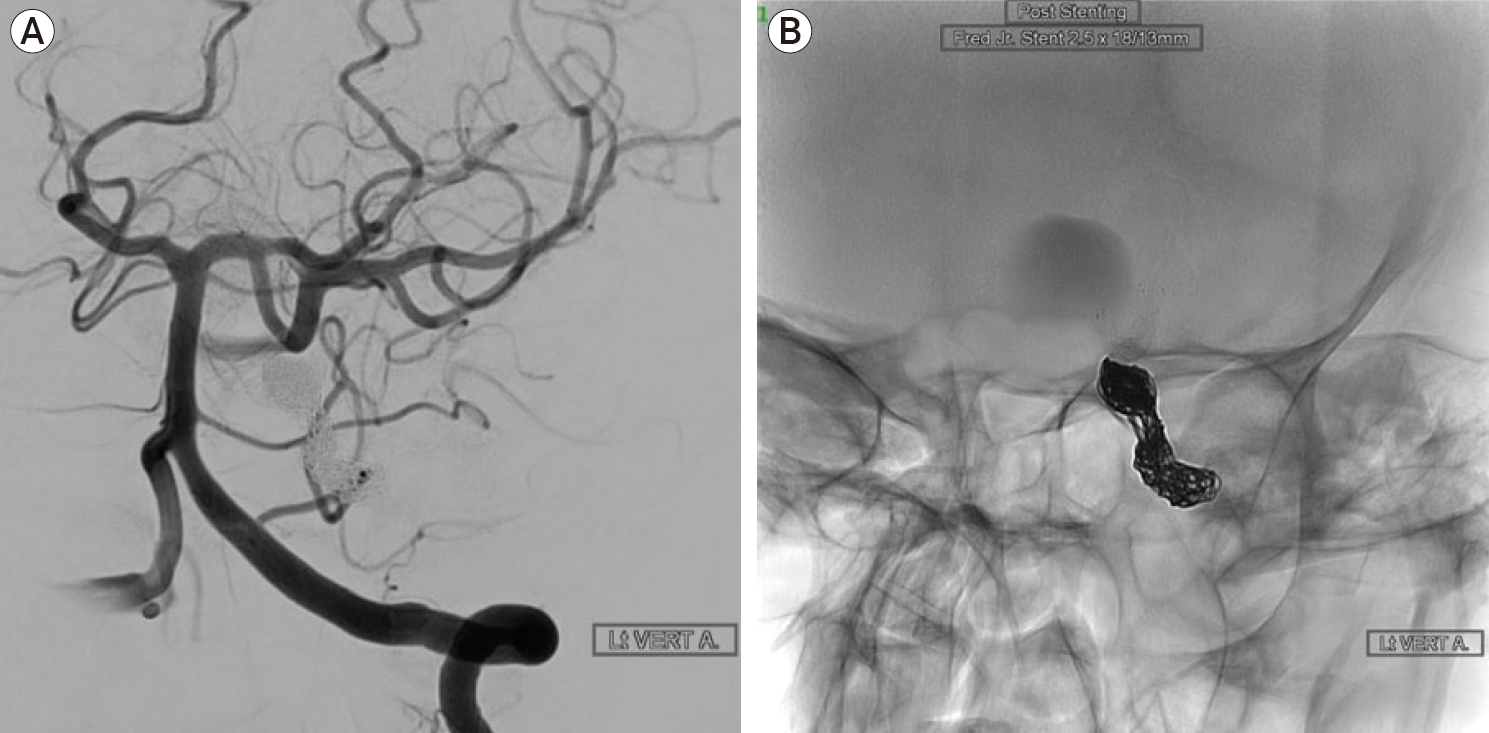
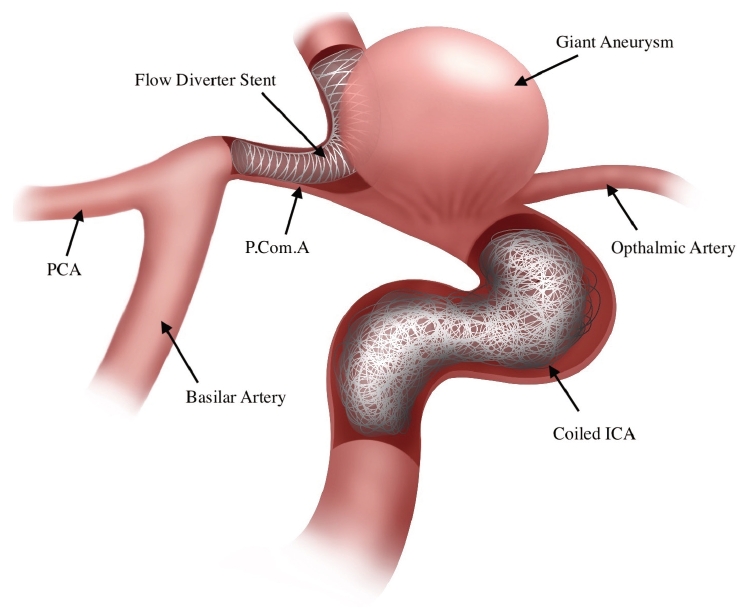
A 54-year-old female, who was found to have incidental giant left ICA aneurysm on magnetic resonance imaging (MRI) scan, during the workup for headaches (Fig. 1). There was no history of thunderclap headache or any associated visual or neurologic symptoms to suggest aneurysm rupture. Initial angiogram for evaluation of aneurysm, demonstrated a large left ICA para-ophthalmic aneurysm, measuring around 26├Ś19 mm with a wide neck of 14 mm (Fig. 2). There was a patent anterior communicating artery with brisk cross filling of the left cerebral vasculature from the contralateral right side as well as patent left PCOM artery. Considering the complex anatomy, size of aneurysm and presence of good collaterals with patent anterior and PCOM artery, a plan was made in another hospital to treat the aneurysm with parent vessel occlusion rather than flow diverter stent. Subsequently, the aneurysm was treated in October 2016. Initially, a balloon occlusion test of the left ICA was performed which was negative for any neurological change during 20 minutes of balloon occlusion with blood pressure challenge as well. Subsequently, occlusion of the left ICA proximal to the aneurysm was performed using multiple coils (Fig. 3A, B). There was no antegrade flow into the left ICA after occlusion with a patent flow into the left cerebral hemisphere through a patent anterior and PCOM arteries (Fig. 4A, B). Angiogram of the left vertebral artery after occlusion of left ICA showed retrograde filling of the left ICA para-ophthalmic aneurysm (Fig. 4C, D). This was considered to occlude overtime considering the competing antegrade intracranial flow. Patient remained asymptomatic after the treatment. Follow up angiogram after 6 months and 2 years demonstrated no antegrade flow in the left ICA, however there was persistent filling of the left ICA aneurysm in a retrograde fashion through the PCOM artery (Fig. 5). The aneurysm was followed up for another year and showed no evidence of occlusion with similar retrograde filling through the PCOM artery with no much change in its size. At this stage, considering the persistent filling of aneurysm, treatment was contemplated and the patient was transferred to our institution. She was successfully treated with a flow diverter stent across the PCOM artery into the distal left ICA. Patient recovered well, with no obvious neurological deficit or post-operative complications. Follow up angiogram after six months of flow diverter stent demonstrated patent flow in the PCOM artery with complete occlusion of the aneurysm with no residual filling (Fig 6). Fig. 7 presents an illustration of the final treatment construct.
The patient was started on Aspirin 100 mg once a day and Plavix 75 mg daily, 7 days prior to the procedure. Right common femoral access was obtained using a 6 Fr short sheath. A 6 Fr Chaperon Guide catheter (MicroVention, Aliso Viejo, CA, USA) was placed at the origin of the left vertebral artery. 5000 units of intravenous heparin was given. Subsequently, a 5 Fr SOFIA catheter (MicroVention, Aliso Viejo, CA, USA) was placed through the Chaperon Guide Catheter into the mid basilar artery. Access was secured into the distal left ICA through the patent left PCOM artery using a combination of Headway 21 microcatheter (MicroVention, Aliso Viejo, CA, USA) and 0.014 inch Traxcess wire. Subsequently, a 3 mm├Ś20 mm FRED Jr. flow diverter stent (MicroVention, Aliso Viejo, CA, USA) was placed across the left PCOM artery into the distal left ICA (Fig. 7). There was immediate stasis of contrast in the aneurysm sac after placement of flow diverter stent. Follow up angiogram was performed after 6 months, which showed complete occlusion of the aneurysm with no residual filling of the aneurysm sac or neck. The PCOM artery remained patent with brisk flow into the distal left ICA.
Giant ICA aneurysms are complex vascular lesions which are difficult to treat with open as well as endovascular surgery [6,7]. Parent vessel occlusion is a well-established treatment option for management of such aneurysms [4,8]. This treatment option is particularly advocated in cases with high chance of recurrence after endovascular treatment due to complex anatomy and large size. Although parent vessel occlusion is a relatively simple procedure to occlude antegrade flow into the aneurysm, one of the potential drawbacks in a few cases is persistent retrograde filling of the aneurysm. Bechan et al. suggested that persistent flow from PCOM due to hemodynamic changes after ICA occlusion prevented intraluminal thrombosis of the aneurysm, especially in aneurysm located distal to a prominent PCOM artery [2]. Most of these retrograde fillings are managed conservatively with changes in flow dynamics promoting thrombosis of the aneurysm overtime. Although considered naive, there have been a few reported cases of ruptured aneurysms related to the retrograde filling [5,9]. There is no proposed management strategy to control retrograde flow into the aneurysms treated with parent vessel sacrifice. In this case there was persistent filling of the aneurysm sac three years after the initial treatment with parent vessel occlusion with no evidence of aneurysm thrombosis. Considering the risk of rupture of aneurysm, treatment was necessary, which was achieved with placement of a flow diverter stent across the PCOM artery into the distal ICA.
Flow diverter stents are specially designed stents which alter the flow dynamics into the aneurysm and provide adequate arrest of flow once they epithelialize into the parent vessel. The flow diverter stents have been widely used and have become standard treatment for large and giant ICA aneurysms [1,3]. They are widely used in clinical settings for management of various intracranial aneurysms. Although there have been several studies published for the use of flow diverter stents for treatment of ICA aneurysms, no such report is published for use of flow diverter stents for treatment of retrograde filling aneurysms. Our case highlights a potential treatment strategy for management of retrograde filling of aneurysms after antegrade flow has been occluded with parent vessel occlusion.
Fig.┬Ā1.
MRI scan with contrast demonstrating a giant aneurysm arising from the para-ophthalmic segment of the left ICA. MRI, magnetic resonance imaging; ICA, internal carotid artery.
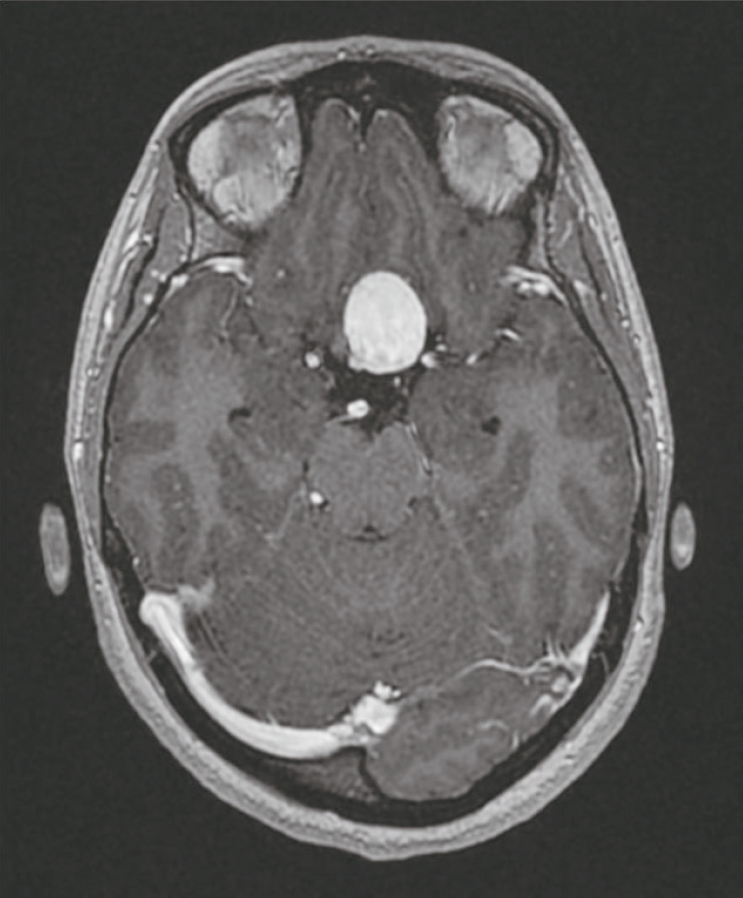
Fig.┬Ā2.
Initial angiogram (A) AP and (B) Lateral views show large left ICA paraphthalmic aneurysm. AP, anteroposterior; ICA, internal carotid artery.

Fig.┬Ā3.
(A) Balloon occlusion test left ICA with balloon inflated in left ICA and angiogram from the right ICA showing brisk filling of the left anterior and middle cerebral artery through a patent anterior communicating artery. (B) Native AP image demonstrating multiple coils used for occlusion of distal left ICA. ICA, internal carotid artery.
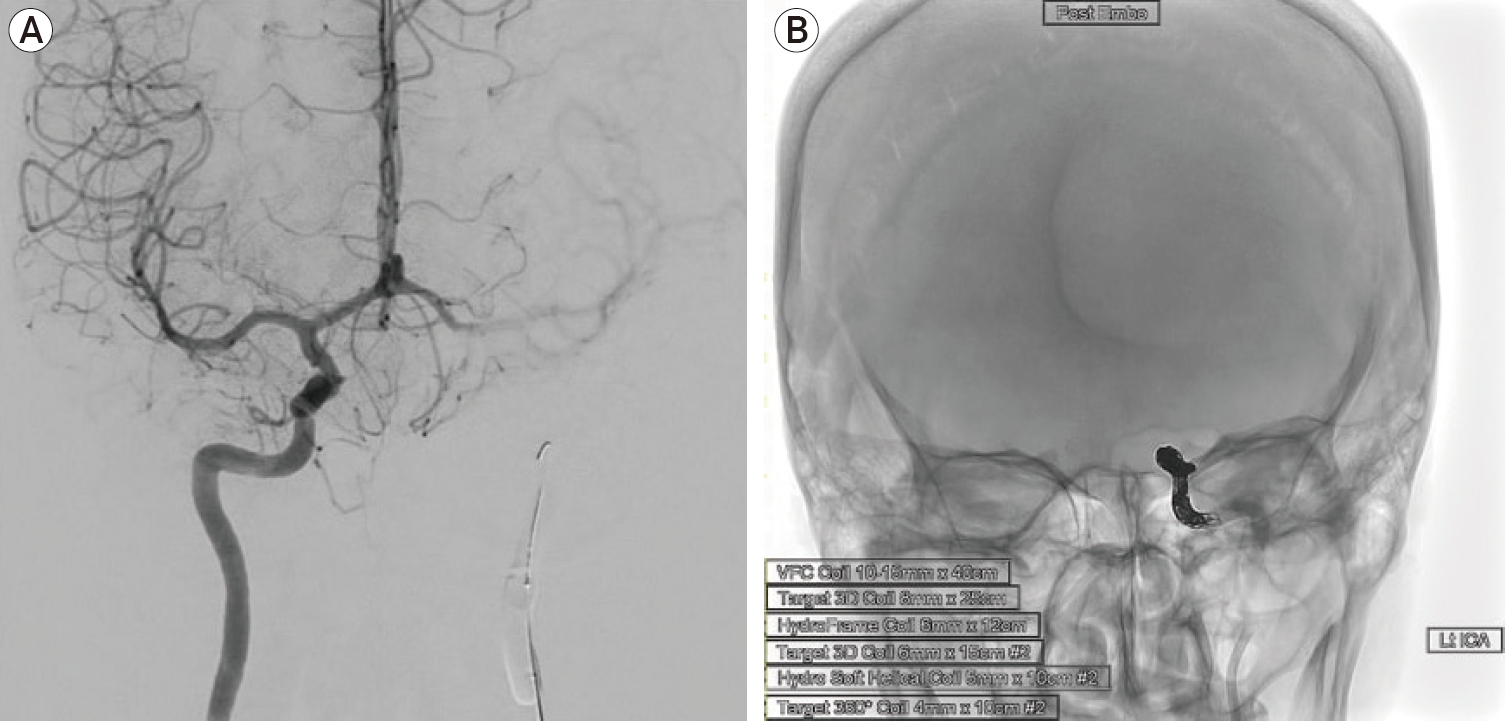
Fig.┬Ā4.
(A) Left ICA AP angiogram demonstrating multiple coils causing occlusion of the distal left ICA with no antegrade filling of the left ICA aneurysm. (B) Right ICA AP angiogram post occlusion of the left ICA shows brisk filling of the left anterior and middle cerebral artery through a patent anterior communicating artery. (C, D) Left vertebral artery AP and Lateral views angiogram shows retrograde filling of the left ICA para-ophthalmic aneurysm after occlusion of left ICA. ICA, internal carotid artery; AP, anteroposterior.
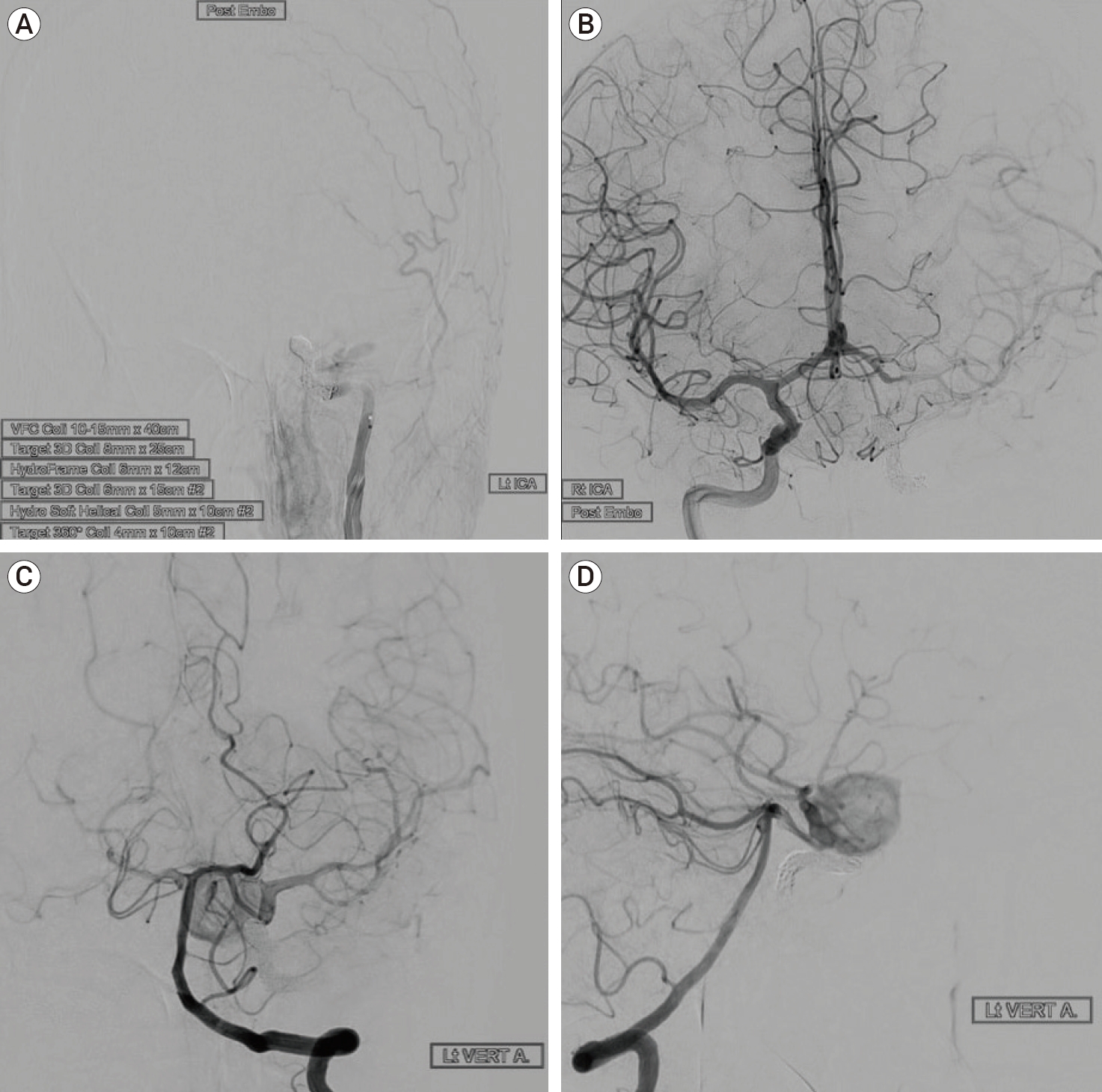
Fig.┬Ā5.
(A) Oblique left vertebral angiogram demonstrates filling of the left ICA aneurysm through a patent left PCOM artery. (B) Oblique native image demonstrating the flow diverter stent across the PCOM artery into the distal left ICA terminating below the carotid terminus. ICA, internal carotid artery; PCOM, posterior communicating.
REFERENCES
1. Adeeb N, Griessenauer CJ, Shallwani H, Shakir H, Foreman PM, Moore JM, et al. Pipeline embolization device in treatment of 50 unruptured large and giant aneurysms. World Neurosurg. 2017 Sep;105:232-7.


2. Bechan RS, Majoie CB, Sprengers ME, Peluso JP, Sluzewski M, Van Rooij WJ. Therapeutic internal carotid artery occlusion for large and giant aneurysms: A single center cohort of 146. Am J Neuroradiol. 2016 37(1):125-9.


3. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013 Jun;267(3):858-68.


4. Cui L, Peng Q, Ha W, Zhou D, Xu Y. Parent artery occlusion for intracranial aneurysms. Interv Neuroradiol. 2009 Sep;15(3):309-15.



5. Gurian JH, Vi├▒uela F, Gobin YP, Waston VE, Duckwiler GR, Gulielmi G. Aneurysm rupture after parent vessel sacrifice: treatment with Guglielmi detachable coil embolization via retrograde catheterization: case report. Neurosurgery. 1995 Dec;37(6):1216-20; discussion 1220-1.

6. Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol. 2003 Feb;24(2):257-62.


7. Solomon RA, Fink ME, Pile-Spellman J. Surgical management of unruptured intracranial aneurysms. J Neurosurg. 1994 Mar;80(3):440-6.


- TOOLS
-
METRICS

-
- 1 Crossref
- 0 Scopus
- 3,717 View
- 88 Download
- ORCID iDs
-
Abdulrahman Y. Alturki

https://orcid.org/0000-0002-1689-9247 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



