 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 19(3); 2017 > Article |
|
Abstract
Currently, endovascular coiling is a popular treatment for basilar tip aneurysms, which usually involve a wide neck. Serious complications can occur when the posterior cerebral artery (PCA) originating from a wide neck is not properly preserved. Accordingly, various adjunctive procedures using stents or a balloon have been introduced. Herein we report two cases of basilar tip aneurysms in which retrograde horizontal (from one PCA to the other PCA) stent-assisted coiling was successful, and we provide a summary of the important technical points.
A large basilar tip aneurysm is usually characterized as a wide-neck aneurysm. If the posterior cerebral artery (PCA) originating from the wide neck is not properly preserved, serious complications, including thalamic infarction can occur. In such cases, preservation techniques using a stent(s) or balloon can be attempted. Y-stents, waffle-cone stents, and horizontal stents may be selected, depending on the angioarchitecture and aneurysmal morphology.1)3)4)5) If a horizontal stent is used, the tortuosity and size of the posterior communicating artery (P-com) should be considered, as stent advancement through the P-com is mandatory. The horizontal stenting trajectory is a long-distance transport from the internal carotid artery (ICA) with a wide P-com to the contralateral P1 segments; thus, various anatomic characteristics should be evaluated thoroughly. Accordingly, horizontal stent-assist coil embolization is not a popular procedure for basilar tip aneurysms. However, horizontal stenting has advantages over other stenting methods, and a retrograde or anterograde approach can be used.8) Herein, we report two cases of basilar tip aneurysms with a wide neck, successfully treated with retrograde horizontal stent-assist coil embolization.
A 56-year-old man presented with stupor and was taken to the emergency room. His Glasgow Coma Scale score (GCS) was E2V1M5. A brain computed tomography (CT) scan taken immediately after admission showed a Fisher grade 3 subarachnoid hemorrhage. A ruptured large basilar tip aneurysm was confirmed on brain CT angiography, and subsequent subtraction catheter cerebral angiography confirmed a saccular basilar tip aneurysm with a wide neck and daughter sac (neck, 6.3 mm; width, 7.7 mm; height, 9.1 mm) (Fig. 1A). The left posterior communicating artery (P-com) was patent and well-developed, with a thickness of 1.9 mm (Fig. 1B).
Stent-assisted coiling was planned and an L-tube was inserted. Because the P-com was prominent on left ICA angiography, we determined it would be possible to reach the left P1 through the P-com. Thus, the left femoral artery was additionally punctured, and an Envoy guiding catheter (Codman & Shurtleff Inc., Raynham, MA, USA) was advanced up to the high cervical portion of the left ICA. The previously inserted Envoy guiding catheter from the right femoral artery was securely advanced up to the mid-V2 portion of the left vertebral artery (VA). The aneurysm had ruptured; thus, heparinization was only performed as an irrigation fluid additive. After simultaneous dye injection through both Envoy catheters, we successfully obtained the roadmap of the anterior to posterior circulation. To pass the Enterprise stent, a Prowler Select Plus (PSP) microcatheter (Codman & Shurtlett, Inc.) was carefully inserted into the left P-com under the guidance of a Traxcess guidewire via the left Envoy. After advancement of the PSP microcatheter to the ending point of the P-com (the junction with the PCA), the Traxcess had to be advanced to the far distal portion of the right PCA to allow maximal safe guidance. The two main obstacles were the “retrograde advancement” into the left P1 and “safe crossing” of the aneurysm neck without violation of aneurysmal sac itself. After many attempts, we successfully advanced the Traxcess, and then the PSP microcatheter, into the right. distal PCA (Fig. 1C). Two Excelsior pre-shaped 45-degree microcatheters (Stryker Neurovascular, Fremont, CA, USA) were inserted into the aneurysmal sac via the right femoral guiding system (through the VA). An Enterprise stent (4.5 × 22 mm; Codman & Shurtlett, Inc.) was carefully pushed upward within the PSP microcatheter, and the horizontal stent was successfully deployed (from the right P1 to the left P1, crossing the aneurysmal neck). Coils were then sequentially inserted using two microcatheters (double-microcatheter method) (Fig. 1D).7) On final angiography, both PCAs were fully saved and the aneurysm was completely packed with a total of 14 coils (163 cm) (Fig. 1E). No findings of acute infarct were observed on postoperative diffusion magnetic resonance imaging (MRI), and the recovery was uneventful.
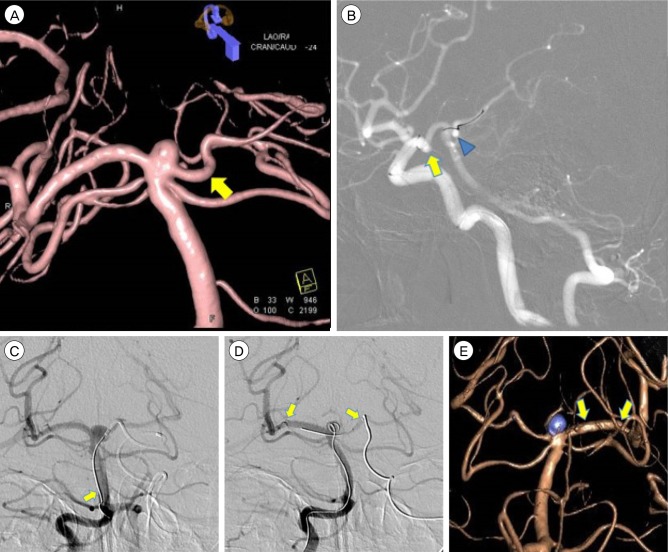
A 69-year-old woman with a history of pontine and myocardial infarctions was admitted for endovascular coil embolization. On admission, she did not present with any specific neurological symptoms. A basilar tip aneurysm was observed on diagnostic cerebral angiography as well as on magnetic resonance angiogram (MRA). The aneurysm (neck, 3.9 mm; height, 2.8 mm; width, 5.3 mm) (Fig. 2A) was shaped like a rugby ball, with an upward direction. The left P-com was 2 mm thick (Fig. 2B).
As the left P-com was thick, horizontal PCA-to-PCA stenting was planned. Both femoral arteries were punctured, and a Shuttle + Envoy system was securely positioned up to the upper V2 portion of the right VA through the right femoral artery and up to the upper cervical portion of the left ICA through the left femoral artery. After the guiding systems were placed securely, the patient was infused with 3,000 units of heparin, followed by an additional 1,000 units per hour. Simultaneous dye injection through both guiding catheters revealed a working angle roadmap from the anterior to posterior circulation. A tentative plan was established to advance a microcatheter through the following path: left P-com → left P1 → right P1 → right distal PCA. We encountered the following technical difficulties.
First, the left P-com had a junctional dilatation origin and acute V-shaped kink, which were obstacles against the stable passage of a microwire. After several changes in tip shape, a Traxcess 14 microwire was delivered to the far distal portion of the left PCA. A PSP microcatheter was then advanced to the junction point between the P-com and PCA (Fig. 2B). Second, the acute, U-shaped angulation of the left P1 made the “retrograde” advancement of a microwire difficult, as the acute horizontal occur immediately after vertical curving of the left P1. To prevent intimal damage, forceful advancement must be avoided; thus, repeated “reshaping” and gentle rotation advancement was performed (Fig. 2B). Third, the U-shaped downward sagging of the left P1 made the “direct” passage of a microwire into the right P1 difficult, as the microwire has a tendency to violate aneurysms with short height. Thus, we passed a microwire into the mid-basilar artery, and then, advanced the microcatheter to the proximal end of the left P1 (Fig. 2C), improving the controllability of the microwire. After several trials, the microwire, and then the microcatheter, was eventually advanced to the right distal PCA without violation of the aneurysm. During microcatheter advancement, delicate tension control with a repeated push-and-pull maneuver was used because of the long, curved trajectory route.
As a jailing technique, an Excelsior SL-10 microcatheter (with vapor-steaming for making extended S-shape) was placed into the mid-point of the aneurysm. The first coil was then partially deployed to reinforce stability. An attempt was made to advance an Enterprise stent (4.5 × 22 mm) using the inserted PSP microcatheter. Despite the use of a Shuttle + Envoy dual-guiding system, severe resistance against stent advancement was noted at the difficult points of microwire passage. To balance the push pressure and friction resistance, a repeated push-and-pull maneuver was inevitable and a strong guiding system was mandatory. Finally, we successfully mounted the Enterprise stent from the right P2 (crossing the aneurysmal neck) to the left P1 (Fig. 2D). Despite the long procedural time, no abnormalities were observed on ICA and VA angiography. Subsequently, coiling was performed through the previously jailed Excelsior microcatheters. The aneurysm was completely packed with a total of 5 coils (21 cm) (Fig. 2E). The patient recovered without any complications, and is currently under follow-up as an outpatient.
The main pitfall in the direct surgical clipping of a basilar tip aneurysm concerns the thalamoperforating arteries, as the visualization and dissection of these perforators are very difficult in some cases of basilar tip aneurysm. The thalamoperforators originate from the proximal PCA (namely, the P1 segment); thus, in cases of coil embolization, the PCAs should also be preserved. Balloon-assisted coil embolization, firstly introduced by Moret et al., shows high rates of delayed coil compaction and aneurysm recurrence.6) Thus, various stenting techniques have been introduced to provide a discrete buttress for coil embolization and scaffolding that diverts blood flow away from aneurysm. Representative stent remodeling techniques include Y stenting and waffle-cone stenting. The Y stenting technique is relatively easy compared to horizontal stenting; however, the probability of thromboembolic complications is higher compared to that with single stents.1) The waffle-cone technique, firstly introduced by Horowitz et al., can warrant the origin of both parent arteries, but the neck itself cannot be blocked.4) Horizontal stenting can meet these two demands with less thrombogenicity and higher neck protection. With basilar tip aneurysms, the anatomic routes (namely, both P-coms) allow an additional horizontal stenting technique, which was firstly introduced by Cross et al.3) This horizontal technique completely depends on P-com anatomy and course, as the horizontal stent is mounted through the P-com. Yashar et al. subsequently described “P-com independent” horizontal stenting, known as antegrade horizontal stenting.8) The access route in this antegrade horizontal stenting technique is actually from the basilar artery to the unilateral PCA, and final stent deployment occurs in a narrow working area between the unilateral PCA and the end of the aneurysm neck or the just-proximal point of the contralateral PCA. Thus, the neck coverage is subordinate to retrograde horizontal stenting, and stent herniation into the aneurysm can occur. In the retrograde technique, a stent is mounted in the bilateral PCAs through the ICA and P-com. This retrograde approach is completely dependent on the thickness of the P-com, and the long route may contain many anatomic and technical pitfalls. However, compared to that in the antegrade technique, the neck coverage is more complete and stable. Thus, to prevent stent miss-lodging and to maximize coil insertion, the retrograde technique is the first choice in the horizontal stenting of basilar tip aneurysms. In the cases reported in the present study, the retrograde approach was used to mount horizontal stents.2) According to a review of reported case studies using an retrograde approach, stenting is attempted if the thickness of the P-com is over 1 mm, and the success rate is high in those cases. As shown in Fig. 2A and 2B, the contrast was clear in the lt. P-com in the present cases. Because the thickness of the lt. P-com was 1.9 mm and 2 mm, respectively, it was easy to move catheters and stents through the P-com. In addition to P-com caliber, equally important point is “angulation” of P-com and P1. Before the application of a horizontal stent, the stable launch of a microwire into the contralateral PCA (through the ipsilateral PCA) is mandatory. In both of the present cases, the left P1 had a downward sagging appearance. However, the passage of the microwire was much easier in Case 1 than in Case 2 for the following reasons: 1) the larger aneurysm permitted the inevitable upward jumping of the microwire, and 2) the upward sagging of the right P1, which has extension line of downward sagging of the left P1. In other words, 1) V-kink of the left P-com of the ICA, 2) short aneurysmal height, 3) much sharper downward sagging of the left P1 caused difficulties in the microwire handling in Case 2. To overcome these obstacles, we introduced a microwire into the proximal basilar artery, advanced the microcatheter, introduced the microwire to the right PCA, and finally launched the microcatheter to the target position.
The present cases highlight that a thorough understanding of the angioarchitecture and flexibility in the procedural strategy are mandatory for the successful deployment of a horizontal stent in basilar tip aneurysms. In summary, to succeed retrograde horizontal stenting for coiling of wide neck basilar tip aneurysm, the main check points and technical summaries are same as follows ; 1) P-com caliber (wider is better), 2) P-com angulation (less acute is better), 3) Both P1 angulations (less acute is better), 4) Aneurysmal size (larger is better)
ACKNOWLEDGEMENTS
We acknowledge that the material is not published previously and would like to thank the Department of Radiology of St Vincent's Hospital, The Catholic University of Korea, Suwon, Korea.
References
1. Akgul E, Aksungur E, Balli T, Onan B, Yilmaz DM, Bicakci S, et al. Y-stent-assisted coil embolization of wide-neck intracranial aneurysms. A single center experience. Interv Neuroradiol. 2011 3;17(1):36-48;



2. Blackburn SL, Kadkhodayan Y, Shekhtman E, Derdeyn CP, Cross DT 3rd, Moran CJ. Treatment of basilar tip aneurysms with horizontal pca to pca stent-assisted coiling: Case series. J Neurointerv Surg. 2013 5;5(3):212-216;


3. Cross DT 3rd, Moran CJ, Derdeyn CP, Mazumdar A, Rivet D, Chicoine MM. Neuroform stent deployment for treatment of a basilar tip aneurysm via a posterior communicating artery route. AJNR Am J Neuroradiol. 2005 Nov-Dec;26(10):2578-2581;


4. Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms: Eight cases using the waffle cone technique. Neurosurgery. 2006 4;58(4 Suppl 2):ONS-258-ONS-262; discussion ONS-262.


5. Liu W, Kung DK, Policeni B, Rossen JD, Jabbour PM, Hasan DM. Stent-assisted coil embolization of complex wide-necked bifurcation cerebral aneurysms using the “waffle cone” technique. A review of ten consecutive cases. Interv Neuroradiol. 2012 3;18(1):20-28;



6. Moret J, Cognard C, Weill A, Castaings L, Rey A. The “remodelling technique” in the treatment of wide neck intracranial aneurysms. Angiographic results and clinical follow-up in 56 cases. Interv Neuroradiol. 1997 3;3(1):21-35;


Fig. 1
Serial angiography images of Case 1. (A) The 3D angiography of case 1 shows saccular aneurysm at basilar tip. The height of aneurysm is about 9 mm. (B) The roadmap view of case 1 shows relatively straight course of left Pcom and PCA. The Pcom size is about 1.9 mm. Compared to case 2, the navigation of microwire (and subsequent) mirocatheter is relatively easy. (C) The roadmap view of case 1 shows one stage navigation of microwire to right distal PCA (arrow). The microcatheter is ready to cross the aneurysm neck. (D) The roadmap view of case 1 shows successful deployment of Enterprise stent (arrows) and subsequent coiling via double microcatheters from left vertebral artery. (E) The final 3D angiography of case 1 shows complete coil packing into aneurysm with excellent preservation of both PCAs. PCA = posterior cerebral artery.
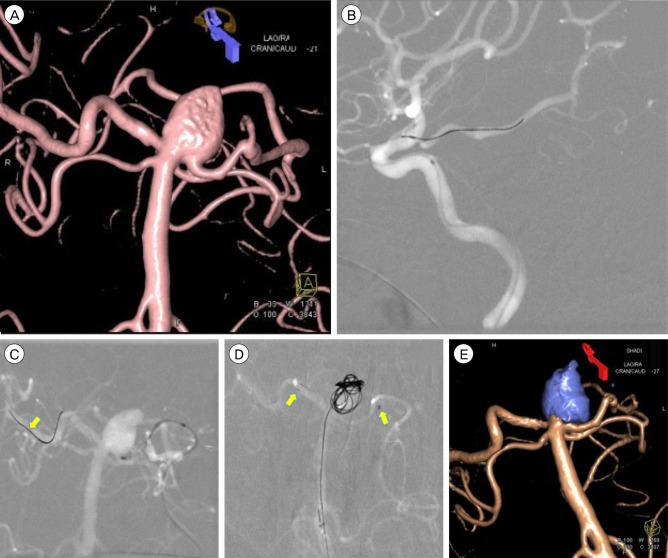
Fig. 2
Serial angiography images of Case 2. (A) The 3D angiography of case 2 shows small saccular aneurysm with at basilar tip. The height of aneurysm is about 2.8 mm. Compared to case 1, note the acute downward sagging course of left P1 segment (arrow), which make subsequent navigation difficult. (B) The roadmap view of case 2 shows V shaped kink of Pcom origin (arrow) and downward sagging of left P1 segment of PCA (triangle). They are big obstacle of navigation of mircowire and catheter. The Pcom size is over 2 mm. (C) The vertebral angiography of case 2 shows two stage navigation of microwire. The acute downward sagging of left P1 and short height of aneurysm make the microwire advance to proximal basilar artery firstly, rather than launch to right PCA directly (arrow). (D) The vertebral angiography of case 2 shows successful deployment of Enterprise stent (arrows) and partially deployed the 1st coil loop into aneurysm sac. After stent deployment, the downward sagging of left P1 is somewhat straightened. (E) The final 3D angiography of case 2 also shows complete packing. The inserted Enterprise stent makes the curved left PCA straight (arrows). PCA = posterior cerebral artery.
- TOOLS
-
METRICS

-
- 4 Crossref
- 0 Scopus
- 2,694 View
- 27 Download
- Related articles
-
Stent-assisted Coil Embolization of Cerebral Aneurysms: Review Article.2011 March;13(1)

 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



