 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 18(2); 2016 > Article |
|
Abstract
We present two patients with a dural arteriovenous fistula (dAVF) of the ophthalmic sheath who developed progressive exophthalmos, conjunctival chemosis, and visual loss. These symptoms mimic those of cavernous sinus dAVFs. Dural AVFs of the ophthalmic sheath are extremely rare and their clinical management is controversial. We successfully treated these two patients by transvenous coil embolization. Transvenous embolization appears to be a safe and effective method to treat dAVFs of the ophthalmic sheath.
Dural arteriovenous fistulas (dAVFs) of the ophthalmic sheath without involvement of the cavernous sinus are extremely rare. To the best of our knowledge, fewer than 20 cases have been reported in the literature.1)2)3)4)5)6)7)8)9)10)11) Because of the small number of reported cases, diagnosis is difficult and treatment methods are controversial.11) We report two cases of dAVFs of the ophthalmic sheath that were treated successfully with transvenous coil embolization and discuss the nature and management of this disease.
A 50-year-old male visited our institute for progressive proptosis, conjunctival chemosis, and worsening of visual acuity during the previous 6 months. He also complained of headache and nausea for 1 week. The patient had no history of head trauma or underlying disease such as diabetes, thyroid disease, or antithrombin III deficiency. On admission, physical examination showed marked conjunctival chemosis and mild proptosis. Bruits were not detectable. Static quantitative perimetry revealed decreased visual acuity in his left eye (20/40) relative to his right (20/20) eye without field defects.
Brain MR imaging showed left superior ophthalmic vein (SOV) engorgement (Fig. 1).
The patient underwent conventional angiography for a definite diagnosis. Cerebral angiography confirmed the presence of a dural AVF of the left ophthalmic sheath with fine feeders from the ophthalmic artery and meningohypophyseal trunk (MHT). Two feeders of the fistula drained the cavernous sinus via the SOV. There was no fistula between the carotid artery and cavernous sinus (Fig. 2).
To relieve the patient's progressive visual symptoms we performed endovascular embolization under general anesthesia. We placed a guiding catheter in the left internal jugular vein and advanced the microcatheter via the inferior petrosal sinus (IPS).8) Because of the tortuous venous structure from the cavernous sinus to the fistula point, access to the fistula point was not easy. Finally, we accessed the fistula point and performed embolization using detachable coils. Post-procedural angiography revealed that the fistula point was occluded, and feeders to the ophthalmic sheath and MHT were not observed (Fig. 3). There were no procedure-related complications. A few days after the procedure, chemosis and proptosis had decreased and both headache and nausea had greatly improved. Static quantitative perimetry revealed that visual acuity in the left eye (20/30) had improved relative to that before the procedure (20/40). The patient did not develop symptoms or signs suggestive of recurrence over a 4-month follow-up period.
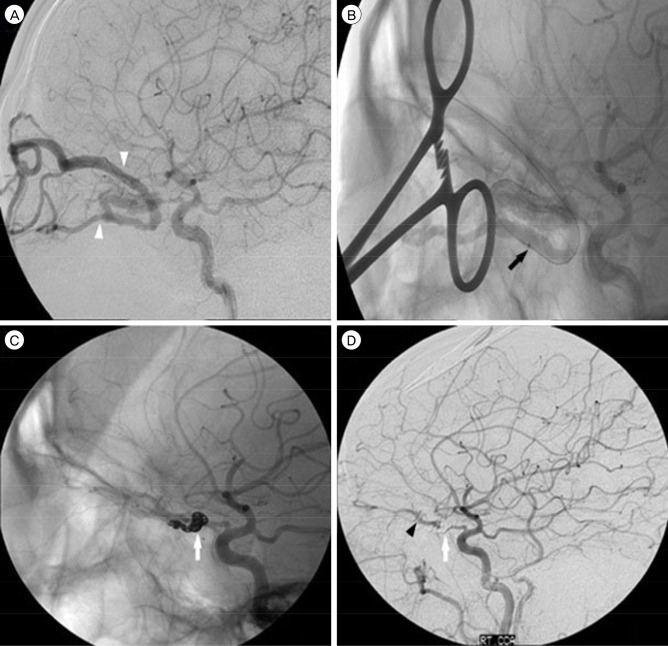
A 55-year-old male presented with progressive proptosis, conjunctival chemosis, and worsening of visual acuity during the last 5 years. Worsening proptosis and conjunctival chemosis prompted him to visit our institution. The patient had a history of right eye trauma in his early years but no history of underlying disease. On admission, the patient's right-sided visual acuity was 20/100 and his left-sided visual acuity was 20/40. Kinetic quantitative perimetry revealed a cecocentral scotomatous defect in the right visual field. Brain MR imaging showed right SOV engorgement. Cerebral angiography confirmed the presence of a dural AVF of the left ophthalmic sheath with a fine feeder from the ophthalmic artery. The feeder of the fistula drained into the superior and inferior ophthalmic veins (Fig. 4).
Transvenous embolization was planned under general anesthesia. Because of the acute angle of the venous structure at the cervical, access to the fistula point was not easy via the angular vein. We therefore embolized the dural AV fistula via direct puncture. The ophthalmologist exposed the SOV. We punctured the SOV and inserted the dilator into the deep portion of the SOV. Finally, we were able to access the fistula point and performed embolization using detachable coils. In post-procedural angiography, the fistula point was occluded and feeders of the ophthalmic sheath were not observed (Fig. 4). There were no procedure-related complications.
A few days after the procedure, chemosis and proptosis had decreased. Visual acuity in the right eye (20/63) had also improved relative to that before the procedure (20/100). At the 1-year follow-up after embolization, the visual field defect in the right eye had improved based on kinetic quantitative perimetry assessment.
Dural AVFs of the ophthalmic sheath can clinically mimic cavernous sinus dAVFs and are associated with ocular findings of chemosis, exophthalmos, and loss of visual acuity.11) A dural arteriovenous fistula of the ophthalmic sheath must be distinguished from a cavernous sinus dAVF. If a dural arteriovenous fistula of the ophthalmic sheath is misdiagnosed as a cavernous sinus dAVF, an incorrect shunting point could be embolized. This incorrect management could in turn increase ophthalmic reflux and aggravate disease. In the two cases described here, we suspected a cavernous sinus dAVF because of clinical features and ophthalmic vein engorgement on brain MR imaging. Patient 1 was more difficult to diagnose than patient 2 because the shunting point was close to the cavernous sinus based on brain MR imaging. Cerebral angiography confirmed the presence of a fistula between the ophthalmic artery and SOV of the ophthalmic sheath. Therefore, to establish an optimal treatment strategy precise diagnosis using catheter angiography is necessary.
There are several treatment options for dural AVFs of the ophthalmic sheath. Recently, surgical removal of the dAVF and transvenous embolization were used to manage the dAVF. Direct surgical removal or obliteration by means of a frontoorbital approach fully restored vision and corrected proptosis.4)5)6) No evidence of recurrence of dAVFs has been found in previous surgical cases.5)10) Therefore, surgical treatment is an effective treatment method, but it is invasive and there are also case-specific risks. Direct surgical removal may be very difficult because of the presence of intraorbital fat, which can obscure structures and is consequently associated with a high risk of hemorrhage.4) A few reports concerning intraorbital dAVFs have advocated transvenous embolization, and some clinicians recommend this as the first choice when treating intracranial dAVFs. Transvenous embolization could reduce the risk of injury to the ophthalmic artery.7)11)
Intraorbital AVFs are an exceptionally rare subtype of AVF, with fewer than 20 cases reported in the literature.1)2)3)4)5)6)7)8)9)10)11) In previous studies, de Keizer3) and Cheng et al.2) reported patients who were managed conservatively by clinical observation and measurement of ocular pressure. Ten cases were successfully managed; however, one case had a poor visual outcome and another case died after angiography.
Hamada et al.5) and Wigton et al.10) described treatment of dAVFs of the ophthalmic sheath by open surgery. They used surgical treatment because both arterial and venous attempts to cannulate the fistula were unsuccessful. Deguchi et al.4), Caragine et al.1), and Williamson et al.11) reported treatment with transvenous coil embolization and recommended this approach as effective and safe. Subramanian et al.9) recommended transvenous coil embolization of an intraorbital AVF using direct cannulation of the SOV via open surgical exposure in the absence of communication between the SOV and the cavernous sinus.
Our two patients were successfully treated with transvenous embolization. Dural AVFs of the ophthalmic sheath can be effectively treated with transvenous embolization, which is less invasive than open surgery. If the detachable coil is not properly positioned, the operator can remove it and reposition it or choose another size of coil. However, an accurate transvenous approach via the IPS or facial veins can be difficult because these veins might be tortuous as a result of pressure-related changes. Furthermore, accurate embolization at the origin of the shunt from the feeding artery to the draining vein is not easy. If a transvenous approach via the IPS or the facial vein is hindered by anatomic limitations, direct cannulation of the SOV may be a viable option.
Symptoms and radiologic findings of ophthalmic sheath AVF can mimic those of a cavernous sinus dAVF.11) Precise conventional angiography is essential for proper diagnosis and treatment. Transvenous embolization appears to be a safe and effective treatment method for direct arteriovenous fistulas of the ophthalmic sheath. If approach via the IPS or facial veins is not feasible, direct cannulation of the SOV can be used as an alternative approach.
References
1. Caragine LP Jr, Halbach VV, Dowd CF, Higashida RT. Intraorbital arteriovenous fistulae of the ophthalmic veins treated by transvenous endovascular occlusion: technical case report. Neurosurgery. 2006 2;58(1 Suppl):ONS-E170.discussion ONS-E170.



2. Cheng KC, Chang CH, Lin WC. Spontaneous resolution of intraorbital arteriovenous fistulas. Ophthal Plast Reconstr Surg. 2009 May-Jun;25(3):245-247.


3. de Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit. 2003 6;22(2):121-142;


4. Deguchi J, Yamada M, Ogawa R, Kuroiwa T. Transvenous embolization for a purely intraorbital arteriovenous fistula. Case report. J Neurosurg. 2005 10;103(4):756-759;


5. Hamada J, Morioka M, Kai Y, Sakurama T, Kuratsu J. Spontaneous arteriovenous fistula of the orbit: case report. Surg Neurol. 2006 1;65(1):55-57; discussion 57.


6. Hieu PD, Besson G, Roncin S, Nonent M. Successful surgical treatment of intraorbital arteriovenous malformations: case report. Neurosurgery. 1997 3;40(3):626-631;


7. Kim AW, Kosmorsky GS. Arteriovenous communication in the orbit. J Neuroophthalmol. 2000 3;20(1):17-19;


8. Levy Z, Satti S, Grillo A. Intercavernous carotid artery aneurysm. J Emerg Med. 2014 2;46(2):e63-e64;


9. Subramanian PS, Gailloud PH, Heck DV, Tamargo RJ, Murphy KJ, Miller NR. Cook detachable coil embolization of a symptomatic, isolated orbital arteriovenous fistula via a superior ophthalmic vein approach. Neuroradiology. 2005 1;47(1):62-65;



Fig. 1
Frontal (A) and superior (B) 3D TOF MRA maximum-intensity projections show a dilated left superior ophthalmic vein (white arrow). TOF MRA = time-of-flight magnetic resonance angiography.
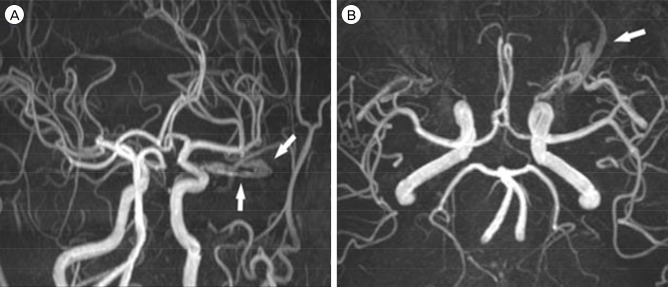
Fig. 2
Lateral projection of left internal carotid angiogram shows dura AVFs of the left optic sheath (white arrow) with fine feeders from the ophthalmic artery and meningohypophyseal trunk (white arrowheads) (A, B). Left optic sheath dural AVF is shown to drain into the cavernous sinus (black arrow) (C). AVF = arteriovenous fistula.
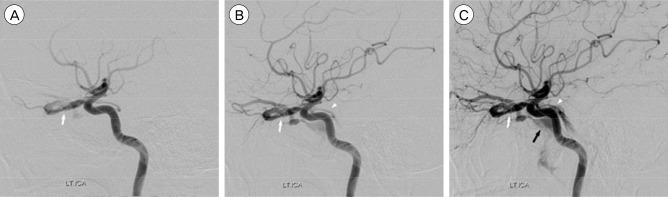
Fig. 3
Angiogram shows the first coil (white arrowhead) inserted into the fistula point of the ophthalmic sheath in lateral view (A) and the fifth coil (white arrowhead) inserted into the shunting point via a transvenous approach. Microcatheter in the superior ophthalmic vein (white arrow) is seen on the lateral view (B) and the AP view (C). Angiogram after embolization shows complete obliteration of left optic sheath dural AVF (white arrowhead) and preserved ophthalmic artery (black arrow) (D). AVF = arteriovenous fistula.
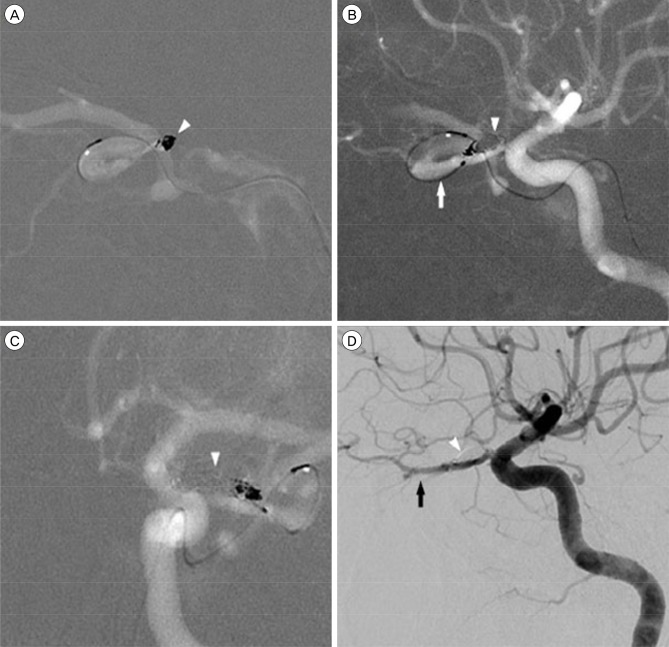
Fig. 4
Angiogram shows dural AVF in the right optic sheath with feeders draining into the superior and inferior ophthalmic veins (white arrowhead) (A). Catheter is directly inserted into the superior ophthalmic vein (black arrow) (B). Coil is inserted into the fistula point of ophthalmic sheath in lateral view (white arrow) (C). Angiogram after embolization shows complete obliteration of right optic sheath dural AVF (white arrow) and preserved ophthalmic artery (black arrowhead) (D). AVF = arteriovenous fistula.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




