 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 19(4); 2017 > Article |
|
Abstract
Objective
We aimed to introduce our method involving prepuncture ultrasound scan for cannulation of the common femoral artery (CFA) during transfemoral cerebral angiography (TFCA), and to assess the clinical and radiological outcomes.
Material and Methods
Our study included 90 patients who underwent prepuncture ultrasound examination of the inguinal area for TFCA between April 2015 and June 2015. Prior to skin preparation and draping of the inguinal area, we identified the CFA and its bifurcation using ultrasound. Based on the ultrasound findings, we marked cruciate lines in the inguinal area. Thereafter, we inserted a puncture needle at the interface between the horizontal and vertical lines at a 30-45┬░ angle, simultaneously palpating the pulsation of the femoral artery. After TFCA was completed, femoral artery angiography was performed in the anteroposterior and oblique directions. Clinical and radiological parameters, including CFA cannulation, the ultrasound scan time, the first pass success rate, the time required for the passage of the wire, and complications, were evaluated.
Results
The mean ultrasound scan time of the CFA and its bifurcation was 72.6 seconds, and the mean time between administration of local anesthesia and wire passage was 67.44 seconds. The first pass success rate was 77.8% (70/90 patients), and the CFA puncture rate was 98.8% (89/90 patients). Although minor complications were noted in 7 patients, no patient reported serious complications (a large hematoma [Ōēź 5 cm], pseudoaneurysms, dissection, and/or a retroperitoneal hematoma.)
The most common complications associated with of diagnostic catheterization performed via the femoral approach are vascular access site complications, which have been reported in 0.44-1.8% of cases.5)14)19) Although various factors influence the complication rate associated with transfemoral angiography; including age, female sex, high body mass index (BMI), and the use of anticoagulants and/or antiplatelet agents.4)24) Reportedly, the most common cause of vascular complications is inappropriate localization of the access site.6) Reportedly, cannulation of the common femoral artery (CFA) has reduces the risk of severe vascular complications because of the size and easy compressibility of this artery.6)11)13) However, cannulation attempted at a site above the inguinal ligament might result in retroperitoneal hemorrhage8)9)13)19)21)23) while cannulation below the site of the CFA bifurcation might result in formation of pseudoaneurysms, arteriovenous fistula, puncture site hematoma, and/or limb ischemia.3)5)13)15)23)
Access to the CFA is important; however, it can sometimes be difficult. To increase the possibility of accurate CFA cannulation, several methods involving the use of anatomical landmarks,11) fluoroscopy,7)12) or real-time ultrasonography1)16)18) have been proposed. Each method is associated with definite advantages and disadvantages, and the most appropriate method to identify an accurate and safe puncture point remains controversial.
We aimed to introduce our novel method involving prepuncture ultrasound examination for cannulation of the CFA during transfemoral cerebral angiography (TFCA), and to assess the clinical and radiological outcomes associated with this method.
This retrospective study included patients who underwent prepuncture ultrasound examination of the inguinal area for TFCA between April 2015 and June 2015 at our hospital. We investigated 149 consecutive patients who underwent TFCA during the study period. We excluded patients in whom the ultrasound scan time or the time between puncture and wire passage was not checked (n = 55) and patients who did not undergo complete examination (n = 4, absence of intraprocedural images for CFA evaluation [n = 1] or postprocedural femoral angiography [n = 3]). Therefore, 90 patients were finally included in this study. We reviewed the medical records of these patients and obtained baseline information (age and sex), medical history (BMI, hypertension, diabetes mellitus [DM], and hyperlipidemia), and information regarding postprocedural complications.
Prior to skin preparation and draping of the inguinal area for TFCA, all patients underwent ultrasound examination of the groin region to identify the anatomical relations and course of the CFA, femoral bifurcation, and superficial and deep femoral arteries (Fig. 1A, B). Based on our ultrasound findings, we marked cruciate lines in the inguinal area. The transverse line represented the level of the femoral bifurcation and the vertical line represented the direction of the CFA (Fig. 1C). After draping the inguinal area, we placed a radiopaque device at the junction of the cruciate lines and confirmed the relationship between the femoral head and femoral artery bifurcation, which had been confirmed using ultrasound, using fluoroscopy (Fig. 1D, E). Next, we advanced an 18-gauge puncture needle from the interface between the horizontal and vertical lines at a 30-45° angle, simultaneously palpating the pulsation of the femoral artery. The femoral artery puncture point was confirmed using fluoroscopy after guide-wire passage (Fig. 1F, G). All fluoroscopic images were obtained in the anteroposterior (AP) and oblique 60-degree directions. The ultrasound scan time, time between administration of local anesthesia and guide-wire passage, and the number of needle advances were recorded by the angiography room staff. After TFCA was completed, we applied a pneumatic pressure-assisted closing device (God's Hand® Plus Pad, MCD Co., Goyang, Korea) to the inguinal area in all patients.
All patients included in this study underwent femoral angiography in the AP and oblique directions after cerebral angiography. Femoral angiographic images were retrospectively reviewed by the authors who were blinded to the clinical information of patients to identify the puncture point, virtual line of the inguinal ligament, locations of the CFA bifurcation and sheath placement, and to measure the diameter and length of the CFA, and the distance between the CFA and the puncture point (Fig. 2). The CFA diameter was measured around the puncture point. The CFA length was measured from a virtual line between the anterosuperior iliac spine and the pubic tubercle (which represented the inguinal ligament) to the femoral bifurcation. As proposed by Yaganti el al.23), we divided the femoral zone into 4 equal zones (zones 1-4) from the upper to the lower margin. Additionally, zone 0 was defined as the area above the upper margin and zone 5 was defined as the area below the lower margin of the femoral head (Fig. 1D, E). CFA bifurcation in zones 0-2 was considered a high bifurcation.
We used the Student's t-test or the Mann-Whitney U test for continuous variables and the Žć2 test or the Fisher exact test for categorical variables to perform univariate analysis. Multivariate logistic regression analysis was performed to predict potential risk factors. All statistical analyses were performed using the SPSS version 17 (IBM SPSS, Chicago, IL, USA) software. A p-value < 0.05 was considered statistically significant.
Of the 90 patients enrolled in this study, 35 (38.9%) were men and 55 (61.1%) were women. The mean ages of men and women were 58.80 ┬▒ 13.85 years and 56.42 ┬▒ 15.01 years, respectively, and the difference was not statistically significant. Additionally, the mean BMI and the incidence of hypertension, DM, and hyperlipidemia were not significantly different between men and women (Table 1).
Intraprocedural clinical and angiographic results are presented in Table 2. The mean ultrasound scan time in all patients was 70.63 ┬▒ 21.54 s, which was not statistically different between men and women. The number of needle advances and the mean time between administration of local anesthesia and wire passage were significantly higher in women than in the men. (1.20 ┬▒ 0.47 vs. 1.45 ┬▒ 0.96 times, p = 0.016 and 36.74 ┬▒ 9.87 vs. 67.44 ┬▒ 105.16 s, p = 0.036, respectively). The mean CFA diameter and mean CFA length were significantly lower in women than in the men (6.31 ┬▒ 1.20 vs. 6.99 ┬▒ 1.05 mm, p = 0.007 and 46.14 ┬▒ 10.27 vs. 54.54 ┬▒ 10.17 mm, p < 0.001, respectively). The CFA bifurcation was observed to be below zone 3 in most patients (91.1%, 82/90 patients). However, 8 patients (8.9%) showed a high CFA bifurcation located between zone 0 and 2. The mean distance between the CFA bifurcation and the puncture point was 19.94 ┬▒ 6.11 mm. The sheath was placed within the CFA in 98.8% (89/90) of the patients. In 1 patient, we inserted the sheath into the deep femoral artery, because we misidentified the branching point of the lateral circumflex artery from the deep femoral artery as the CFA bifurcation.
Results of univariate and multivariate analyses performed to compare the differences in radiological and clinical characteristics between patients with first pass success and those with first pass failure are summarized in Table 3. Multivariate logistic regression analysis showed that the mean CFA diameter and mean CFA length were greater in patients with first pass success than in those with first pass failure (p = 0.049, odds ratio [OR] 1.827, confidence interval [CI] 1.002-3.329 and p = 0.023, OR 1.065, CI 1.009-1.124, respectively). However, clinical characteristics, including age, sex, hypertension, DM, and hyperlipidemia, were not significantly different between using both univariate and multivariate analyses.
Complications associated with vascular access are presented in Table 4. Complications were reported in 7 (8.9%) patients. 1 patient demonstrated an inguinal hematoma < 5 mm in size, 5 patients demonstrated bruises, and 2 patients complained of pain. All complications were categorized as minor, and no patient reported serious complications such as a large hematoma (Ōēź 5 cm) requiring transfusion, femoral artery pseudoaneurysm and dissection, and/or a retroperitoneal hematoma.
Several methods involving the use of anatomical landmarks,11) standard fluoroscopy,7)12) or real-time ultrasound examination1)16)18) have been proposed to improve the rate of CFA puncture and reduce the risk of complications. Using anatomical landmark guidance, superficial landmarks, including the inguinal skin crease, the maximal femoral pulse, and palpable bony landmarks, have been used to select the site of puncture. This is a simple and basic method; however, it can become challenging in some patients such as those presenting with a feeble pulse and patients with obesity in whom bony landmarks cannot be accurately identified.6) Additionally, using the inguinal crease, which is one of the most popular and preferred landmark might lead to inaccurate result because it is located below the CFA bifurcation in 78% of patients.11) Fluoroscopy-guided CFA cannulation has been proposed to improve the rate of CFA cannulation. This method has been widely used considering that the femoral artery bifurcation occurs below the inferior border of the femoral head in 65% of patients.1)15)17) However, in patients with a feeble pulse, arterial puncture could be challenging and the examination time might be prolonged, which is similar to the limitations noted with use of anatomical landmarks as a guide for cannulation.10)22) Additionally, there is a potential risk of puncture below the CFA bifurcation because the CFA bifurcation is present above the midline of the femoral head (zones 0, 1, and 2) in some patients.2)18) In our study, 8 patients (8.9%) demonstrated a high CFA bifurcation in zone 2 or above. Recently, a few authors have reported that real-time ultrasound guidance might be superior to fluoroscopic guidance.1)18) They reported that CFA puncture using real-time ultrasound guidance was associated with a fewer number of attempts and a shorter median access time, and a higher first pass success rate. Additionally, they reported that this method was useful in patients with a feeble arterial pulse or patients with obesity. However, the CFA cannulation rate was not significantly different between the real-time ultrasound guidance and fluoroscopic guidance techniques. Moreover, improved CFA cannulation was achieved only in patients presenting with a high bifurcation. The primary drawbacks of this method are the additional time required to setup the sterile transducer and difficulties in the maintenance of sterility and management of supplementary equipment.20) Moreover, the complexities associated with use of the method and the inconvenience during use have resulted in low acceptance by interventionists.
Advantages associated with our method: 1) No additional time is required to set up a sterile transducer and related equipment. Ultrasound examination can be easily performed within a short time without requiring sterilization during the preparation of routine angiographic devices for the procedure. 2) Our method can reduce the rate of low puncture, which is similar to the benefit obtained with use of real-time ultrasound guidance because the CFA bifurcation can be confirmed using ultrasound examination prior to needle advancement. In our study, only 1 patient demonstrated a low puncture owing to misreading of ultrasound examination findings. 3) Cruciate skin markings, which represent the direction of the femoral artery and location of the bifurcation can help interventionists optimize the localization of the puncture in conjunction with familiar methods such as anatomical landmark guidance and fluoroscopic guidance. In this study, we achieved accurate CFA cannulation in 98.8% (89/90) of the patients. Additionally, no patient reported serious complications such as a large hematoma, pseudoaneurysms, dissection, and/or retroperitoneal hematoma. Our results showed that performing an ultrasound examination prior to CFA puncture to evaluate the location of the CFA and its bifurcation could help facilitate accurate and safe CFA access without serious complications. Moreover, ours is a simple method that can be easily used in a clinical setting.
Limitations of our study: 1) The retrospective design of the study and the small number of patients was a drawback. 2) Additionally, this study was performed at a single hospital. 3) A control group was not included. Further prospective randomized studies with a large number of patients should be performed to confirm our findings.
References
1. Abu-Fadel MS, Sparling JM, Zacharias SJ, Aston CE, Saucedo JF, Schechter E, et al. Fluoroscopy vs. traditional guided femoral arterial access and the use of closure devices: a randomized controlled trial. Catheter Cardiovasc Interv. 2009 10;74(4):533-539;


2. Ahn HY, Lee HJ, Lee HJ, Yang JH, Yi JS, Lee IW. Assessment of the optimal site of femoral artery puncture and angiographic anatomical study of the common femoral artery. J Korean Neurosurg Soc. 2014 8;56(2):91-97;




3. Altin RS, Flicker S, Naidech HJ. Pseudoaneurysm and arteriovenous fistula after femoral artery catheterization: association with low femoral punctures. AJR Am J Roentgenol. 1989 3;152(3):629-631;


4. Ammann P, Brunner-La Rocca HP, Angehrn W, Roelli H, Sagmeister M, Rickli H. Procedural complications following diagnostic coronary angiography are related to the operator's experience and the catheter size. Catheter Cardiovasc Interv. 2003 5;59(1):13-18;


5. Chandrasekar B, Doucet S, Bilodeau L, Crepeau J, deGuise P, Gregoire J, et al. Complications of cardiac catheterization in the current era: a single-center experience. Catheter Cardiovasc Interv. 2001 3;52(3):289-295;


6. Chinikar M, Ahmadi A, Heidarzadeh A, Sadeghipour P. Imaging or trusting on surface anatomy? A comparison between fluoroscopic guidance and anatomic landmarks for femoral artery access in diagnostic cardiac catheterization. A randomized control trial. Cardiovasc Interv Ther. 2014 1;29(1):18-23;



7. Dotter CT, R├Čsen J, Robinson M. Fluoroscopic guidance in femoral artery puncture. Radiology. 1978 4;127(1):266-267;


8. Ellis SG, Bhatt D, Kapadia S, Lee D, Yen M, Whitlow PL. Correlates and outcomes of retroperitoneal hemorrhage complicating percutaneous coronary intervention. Catheter Cardiovasc Interv. 2006 4;67(4):541-545;


9. Farouque HO, Tremmel JA, Raissi Shabari F, Aggarwal M, Fearon WF, Ng MK, et al. Risk factors for the development of retroperitoneal hematoma after percutaneous coronary intervention in the era of glycoprotein IIb/IIIa inhibitors and vascular closure devices. J Am Coll Cardiol. 2005 2;45(3):363-368;


10. Gedikoglu M, Oguzkurt L, Gur S, Andic C, Sariturk C, Ozkan U. Comparison of ultrasound guidance with the traditional palpation and fluoroscopy method for the common femoral artery puncture. Catheter Cardiovasc Interv. 2013 12;82(7):1187-1192;


11. Grier D, Hartnell G. Percutaneous femoral artery puncture: practice and anatomy. Br J Radiol. 1990 8;63(752):602-604;


13. Irani F, Kumar S, Colyer WR Jr. Common femoral artery access techniques: a review. J Cardiovasc Med (Hagerstown). 2009 7;10(7):517-522;


14. Johnson LW, Esente P, Giambartolomei A, Grant WD, Loin M, Reger MJ, et al. Peripheral vascular complications of coronary angioplasty by the femoral and brachial techniques. Cathet Cardiovasc Diagn. 1994 3;31(3):165-172;


15. Kim D, Orron DE, Skillman JJ, Kent KC, Porter DH, Schlam BW, et al. Role of superficial femoral artery puncture in the development of pseudoaneurysm and arteriovenous fistula complicating percutaneous transfemoral cardiac catheterization. Cathet Cardiovasc Diagn. 1992 2;25(2):91-97;


16. Maecken T, Grau T. Ultrasound imaging in vascular access. Crit Care Med. 2007 5;35(5 Suppl):S178-S185;


17. Schnyder G, Sawhney N, Whisenant B, Tsimikas S, Turi ZG. Common femoral artery anatomy is influenced by demographics and comorbidity: implications for cardiac and peripheral invasive studies. Catheter Cardiovasc Interv. 2001 7;53(3):289-295;


18. Seto AH, Abu-Fadel MS, Sparling JM, Zacharias SJ, Daly TS, Harrison AT, et al. Real-time ultrasound guidance facilitates femoral arterial access and reduces vascular complications: FAUST (Femoral Arterial Access With Ultrasound Trial). JACC Cardiovasc Interv. 2010 7;3(7):751-758;


19. Sherev DA, Shaw RE, Brent BN. Angiographic predictors of femoral access site complications: implication for planned percutaneous coronary intervention. Catheter Cardiovasc Interv. 2005 6;65(2):196-202;


20. Stegemann E, Stegemann B, Marx N, Lauer T, Hoffmann R. Effect of preinterventional ultrasound examination on frequency of procedure-related vascular complications in percutaneous coronary interventions with transfemoral approach. Am J Cardiol. 2011 11;108(9):1203-1206;


21. Tiroch KA, Arora N, Matheny ME, Liu C, Lee TC, Resnic FS. Risk predictors of retroperitoneal hemorrhage following percutaneous coronary intervention. Am J Cardiol. 2008 12;102(11):1473-1476;


22. Wacker F, Wolf KJ, Fobbe F. Percutaneous vascular access guided by color duplex sonography. Eur Radiol. 1997 11;7(9):1501-1504;



23. Yaganti V, Mejevoi N, Hasan O, Cohen M, Wasty N. Pitfalls associated with the use of current recommendations for fluoroscopy-guided common femoral artery access. Catheter Cardiovasc Interv. 2013 3;81(4):674-679;


24. Yatskar L, Selzer F, Feit F, Cohen HA, Jacobs AK, Williams DO, et al. Access site hematoma requiring blood transfusion predicts mortality in patients undergoing percutaneous coronary intervention: data from the National Heart, Lung, and Blood Institute Dynamic Registry. Catheter Cardiovasc Interv. 2007 6;69(7):961-966;


Fig.┬Ā1
Prepuncture ultrasound images obtained in the angiography room. (A) A transverse view showing the common femoral artery (CFA) bifurcation (white arrow). (B) A longitudinal view showing the CFA (arrowhead) and the CFA bifurcation (white arrow). (C) Cruciate lines are marked on the skin based on the findings of an ultrasound examination. The transverse line indicates the level of the CFA bifurcation (white arrows), and the longitudinal line indicates the direction of the CFA (arrowheads). (D, E) Anteroposterior (D) and oblique (E) views of the radiopaque device placed at the junction of the cruciate lines after draping the inguinal area. The relation between the femoral head and femoral artery bifurcation is confirmed with the images. (F, G) Anteroposterior (F) and oblique (G) views obtained after femoral artery puncture and passage of the guide-wire. The femoral artery puncture point (white arrow) is confirmed using fluoroscopy.

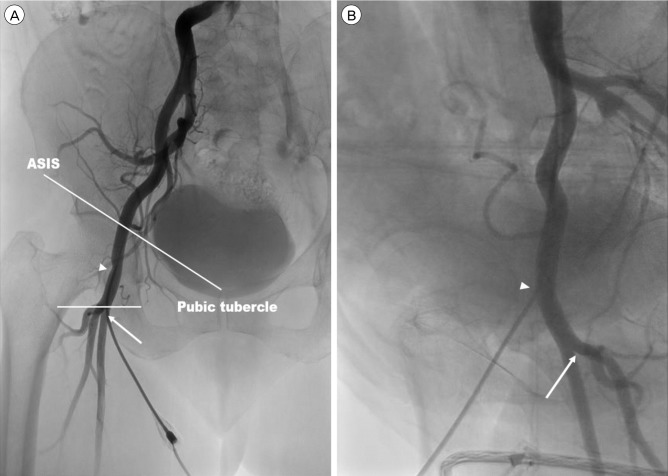
Fig.┬Ā2
Femoral artery angiography images. (A, B) Anteroposterior (A) and oblique (B) views. The virtual line between the anterior superior iliac spine (ASIS) and the pubic tubercle is considered the inguinal ligament. The common femoral artery (CFA) length is measured between the inguinal ligament and the CFA bifurcation (white arrow). The sheath insertion point (arrowhead) is located within the CFA.
Table┬Ā1
Baseline patient characteristics
Table┬Ā2
Intraprocedural clinical and radiological results
Table┬Ā3
Comparison of radiological and clinical characteristics between patients with first pass success and those with first pass failure
- TOOLS
-
METRICS

-
- 3 Crossref
- 0 Scopus
- 3,196 View
- 28 Download
- Related articles




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



