 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 19(3); 2017 > Article |
|
Abstract
The premammillary artery (PMA) is a branch of the posterior communicating artery (PCoA). While the PMA is known to originate from the PCoA as demonstrated by most anatomical studies, it originates directly from the internal carotid artery in approximately 1% of patients. Cerebral aneurysms associated with the PMA have rarely been reported. We report an extremely rare case of a ruptured PMA aneurysm that was managed using endovascular treatment.
The premammillary artery (PMA) is usually the largest and most constant perforating branch of the posterior communicating artery (PCoA) penetrating the area known as the paramedian perforated substance that is situated between the optic tract, mammillary bodies, and cerebral peduncle.4)5)12)13) Few articles have reported the anatomical and functional significance of the PMA,2)3)4) and a few other and a few other studies have reported that it has rarely been observed to directly originate from the internal carotid artery (ICA).2)3) Distally located PMA aneurysms have rarely been reported.6)7)8)10) To our knowledge, no reports in literature have described a ruptured aneurysm involving a PMA directly originating from the ICA. We report a rare case of a patient who presented with this anomaly that was managed using endovascular treatment (EVT).
A 46-year-old man with no significant medical history was transferred to the emergency room with a change in his level of consciousness after the sudden onset of a headache. Upon neurological examination, he was observed to be stuporous mentality. Computed tomography (CT) of the brain demonstrated subarachnoid hemorrhage (SAH) within the basal cisterns with an intra-parenchymal hematoma extending toward the left frontal lobe. Additionally, a CT angiogram demonstrated a fusiform aneurysm involving the communicating segment of the right ICA (Fig. 1). Digital subtraction angiography (DSA) revealed a fusiform aneurysm measuring approximately 4 × 3 mm in its greatest diameter. And no other definite lesions that could account for SAH were noted.
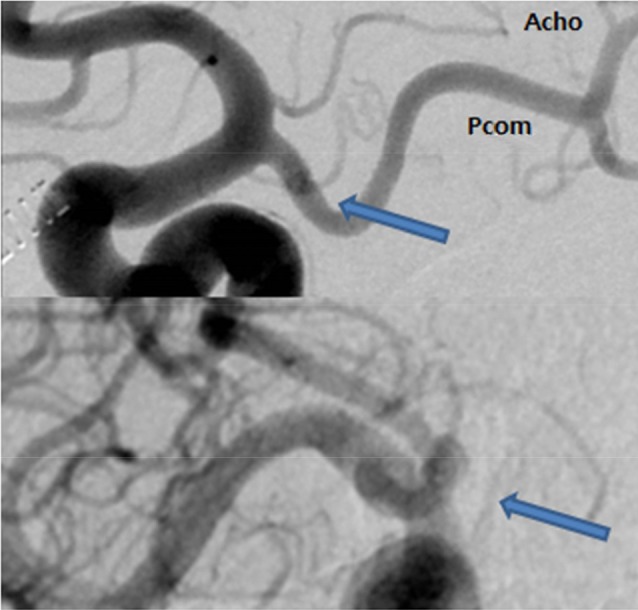
The aneurysm involved the proximal segment of an undefined parent artery originating from the ICA (Fig. 2). Similar to the PCoA and anterior choroidal artery (AChoA), the parent artery originated from the ICA just proximal to the orgin of the PCoA. This artery did not form fenestrations with the PCoA and AChoA, but followed an independent course. Furthermore, the parent artery showed a short distal course running toward the prepontine cistern in a medial-posterior direction. Based on the course of the parent artery, it was determined to be the PMA.
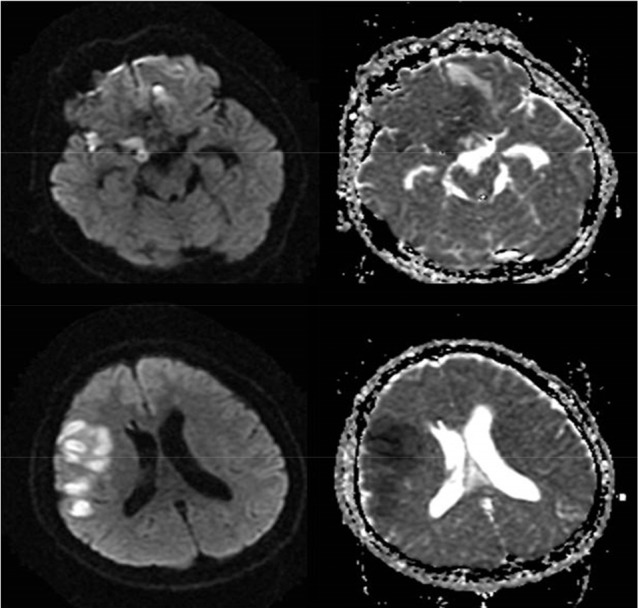
We decided to perform EVT to treat the aneurysm by completely occluding the aneurysmal sac, despite the possibility of causing infarction in the area supplied by the PMA. This procedure was performed under general anesthesia. We inserted a 6 French guiding catheter (Envoy, Cordis, Miami Lakes, FL, USA) into the right distal cervical segment of the ICA. The distal outer diameter of the Excelsior SL-10 microcatheter (Stryker, Fremont, CA, USA) is 0.56 mm. The PMA was shown to be was shown to be 0.7 mm in diameter (measured using DSA). Thus, navigation through the PMA was considered possible. The microcatheter was navigated into the PMA, its tip was positioned in the aneurysm, and the aneurysm was subsequently occluded using 2 detachable coils. Post-coiling angiography showed that the blood flow was maintained in the parent artery (Fig. 3). However, follow-up angiography performed 5 minutes later confirmed complete occlusion of the aneurysm without blood flow through the parent artery. After the procedure, the patient's consciousness improved to a drowsy state but soon worsened to a stuporous state on post operative day (POD) 1. A brain CT scan confirmed the presence of hydrocephalus necessitating the insertion of an external ventricular drain. Follow-up DSA performed on POD 7 demonstrated complete occlusion of the aneurysm, and no other aneurysm and/or vascular malformation was detected. On POD 11, the patient demonstrated right hemiparesis and global aphasia. A transcranial Doppler confirmed increased velocity in the right MCA, which was attributable to post-SAH vasospasm. A diffusion magnetic resonance imaging (MRI) scan showed cerebral infarction in the right hypothalamus and fronto-parietal lobe (Fig. 4). Infarction of the right hypothalamus was secondary to occlusion of the PMA, and infarction of the fronto-parietal lobe was attributed to the vasospasm. Despite these complications, the patient showed complete neurological recovery a month after the EVT.
A PMA aneurysm is an extremely rare condition. A few reports available in literature describe ruptured aneurysms involving this artery. Kumar et al.8) have reported a case wherein a conservative approach effectively treated this condition with follow-up angiography showing disappearance of the aneurysm. However, Kim et al.9) describe using microsurgical clipping to occlude and treat a deep-seated intra-parenchymal aneurysm. Lee et al.10) were the first to describe a case treated with EVT and reported their conclusions: 1) Surgical approaches to PMA aneurysms are difficult because of their deep-seated location in and around the basal ganglia, and 2) EVT is often difficult to perform because of the small caliber, acute angle, and tortuosity of the PMA.
The PMA (also known as the thalamotuberal, tuberothalamic, or the anterior thalamoperforating artery) is the largest branch of the PCoA and penetrates the diencephalon (the floor of the third ventricle) just rosto-lateral to the mammillary bodies. It supplies very important regions of the diencephalon (the hypothalamus, subthalamus, and thalamus), as well as certain parts of the rostral brainstem and occasionally the optic tract.3)4)5)12)13) Because the PMA is an end-artery in most cases, any injury such as a thromboembolic event associated with this vessel leads to neurological sequelae.9) The clinical consequences of a lacunar infarct secondary to PMA occlusion have been described as a specific syndrome characterized by the acute onset of contralateral motor weakness, changes in the superficial modalities of sensation, neuropsychological dysfunction such as apathy, lack of spontaneity, and disorientation, as well as language and memory disturbances.1)2)11) In our patient, occlusion of the PMA after coil embolization was not evident during the acute phase; however, it did lead to cerebral infarction of the area supplied by the PMA, which was detected by diffusion MRI testing performed on POD 11. Neurological deficits such as hemiparesis and dysarthria were considered to be the result of infarction of the fronto-parietal lobe followed by cerebral vasospasm. Hypothalamus infarction noted using diffusion MRI was considered to be masked with mild symptoms or silent infarction in a drowsy mental status.
In terms of its anatomy, the PMA originates from the middle third of the PCoA in 50% of patients, from the anterior third in 17% of patients, and from the posterior third in 13% of patients. In about 1% of patients, the PMA directly originates from the ICA. However, anatomical variations wherein the PMA appears to originate from the ICA may be misleading because the PMA resembles the AChoA resembles the AChoA in terms of diameter, course, and shape. The PMA can be accurately identified and differentiated from the AChoA only by following its course as it runs toward its zone of penetration. To our knowledge, ours is the first case to report a ruptured aneurysm involving the PMA originating directly from the ICA. An optimal treatment strategy has not yet been established for the management of such lesions. Although microsurgical aneurysm clipping may be a feasible option, clipping might be difficult for deep-seated lesions particularly when it is important to preserve the PMA and adjacent perforating artery. In such instances, obliteration of the aneurysm could be achieved through trapping confirmed angiographically. We anticipated complications due to infarction secondary to the anatomical characteristics of the PMA; however, we concluded that total occlusion of the aneurysm achieved through EVT would be beneficial to prevent fatal rebleeding.
We report an extremely rare case of a ruptured PMA aneurysm. EVT can be considered a useful treatment approach for the management of PMA aneurysms that are deep-seated in the brain. However, EVT could be difficult to perform owing to the small caliber of the involved vessels. Additionally, clinicians need to aware of the possibility of infarction of the hypothalamus, subthalamus, and thalamus resulting from total occlusion of the vessels.
References
1. Bogousslavsky J, Regli F, Assal G. The syndrome of unilateral tuberothalamic artery territory infarction. Stroke. 1986 May-Jun;17(3):434-441;


2. Endo H, Sato K, Kondo R, Matsumoto Y, Takahashi A, Tominaga T. Tuberothalamic artery infarctions following coil embolization of ruptured posterior communicating artery aneurysms with posterior communicating artery sacrifice. AJNR Am J Neuroradiol. 2012 3;33(3):500-506;



3. Gabrovsky S, Laleva M, Gabrovsky N. The premammillary artery-a microanatomical study. Acta Neurochir (Wien). 2010 12;152(12):2183-2189;



4. Gibo H, Lenkey C, Rhoton AL Jr. Microsurgical anatomy of the supraclinoid portion of the internal carotid artery. J Neurosurg. 1981 10;55(4):560-574;


5. Gibo H, Marinkovic S, Brigante L. The microsurgical anatomy of the premammillary artery. J Clin Neurosci. 2001 5;8(3):256-260;


6. Kim DS, Yoo DS, Huh PW, Cho KS, Kang JK. Anterior thalamoperforating artery aneurysm associated with internal carotid artery occlusion: case report. Neurosurgery. 1999 10;45(4):911-913;


7. Kownacki JD, Remonda L, Godoy N, Krauss J. Subependymal thalamic haemorrhage due to a thalamoperforating artery aneurysm. J Neurol Neurosurg Psychiatry. 1998 11;65(5):669678



8. Kumar AJ, Zinreich SJ, Preziosi TJ. Rupture of an anterior thalamoperforating artery aneurysm: cause of basal ganglia hemorrhage. AJNR Am J Neuroradiol. 1982 Sep-Oct;3(5):581-582;


9. Kim SH, Yeo DK, Shum JJ, Yoon SM, Chang JC, Bae HG. Morphometric Study of the Anterior thalamoperforating Arteries. J Korean Neurosurg Soc. 2015 5;57(5):350-358;




10. Lee JI, Choi CH, Ko JK, Lee TH. Glue embolization of ruptured anterior thalamoperforating artery aneurysm in patient with both internal carotid arteries occlusion. J Korean Neurosurg Soc. 2011 5;49(5):287-289;




11. Lisovoski F, Koskas P, Dubard T, Dessarts I, Dehen H, Cambier J. Left tuberothalamic artery territory infarction: neuropsychological and MRI features. Eur Neurol. 1993 33(2):181-184;


Fig. 1
Computed tomography (CT) of the brain demonstrating subarachnoid hemorrhage (SAH) within the basal cisterns with an intra-parenchymal hematoma observed extending to the left frontal lobe. A CT angiogram demonstrates a fusiform aneurysm involving the communicating segment of the right internal carotid artery.
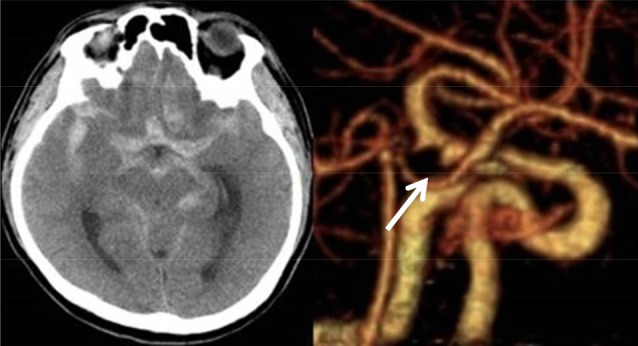
Fig. 2
Digital subtraction angiography (DSA) reveals an aneurysm involving the proximal segment of an undefined parent artery (thick arrows) originating from the internal carotid artery (ICA). The parent artery originates from the ICA just proximal to the origin of the posterior communicating artery (PCoA). This parent artery shows a short course in its distal segment running toward the prepontine cistern in a medial-posterior direction. The artery does not form fenestrations with the PCoA and anterior choroidal artery and follows an independent course.
- TOOLS
-
METRICS

-
- 2 Crossref
- 0 Scopus
- 2,420 View
- 22 Download
- Related articles
-
Endovascular Treatment of Giant Basilar Trunk Aneurysm: Case Report.2001 March;3(1)
Five Aneurysms Arising from the Ipsilateral Internal Carotid Artery : Case Report.2011 March;13(1)





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



